Antibiotics are drugs used to treat bacterial infections. However, antibiotics should only be used in extreme cases - when necessary, as excessive use of them can lead to resistance/resistance of bacteria, making the treatment of future infections particularly difficult and, above all, less effective.
ANTIBIOTICS: What are antibiotics? | Types of infections | Side Effects of Antibiotics | When not to use antibiotics? | Types of antibiotics | Choice of Antibiotics | Interactions | Antibiotic RESISTANCE - the source of ALL PROBLEMS! | Questions and Answers | Sources/references
The word antibiotic means "against life." Antibiotics help stop or treat the development of an infection caused by bacteria in the human body. They do this by preventing the development of bacteria or preventing them from replicating or multiplying. Any drug that kills microbes in the human body is known as an antibiotic.
Before scientists discovered antibiotics for the first time in the 1920s, many people died from minor bacterial infections, such as strep throat, and every operation was also hazardous.

However, when antibiotics became available in the 1940s, life expectancy increased precisely because operations became safer, and people could survive once deadly infections.
What can antibiotics treat, and what can't they?
Most bacteria in your body are harmless; some are beneficial and coexist with you in the digestive tract.
Video content: how do antibiotics work?

Nevertheless, bacteria outside the digestive tract can do a lot of damage and infect almost any organ. Fortunately, antibiotics can help with this very successfully.
These are the types of infections that can be treated with antibiotics
- ear and sinus infections
- infections of the oral cavity
- skin infections
- meningitis (swelling of the brain and spinal cord)
- sore throat
- bladder and kidney infections
- bacterial pneumonia
- whooping cough
- Clostridioides difficile
Only bacterial infections can be treated with antibiotics. Colds, flu, coughs, some bronchial infections, sore throats, and stomach flu are caused by viruses but cannot be eliminated with antibiotics. Unfortunately, antibiotics will not be able to cure them. Unfortunately, it is not always clear whether the infection is viral or bacterial, so quality diagnostics are necessary before starting successful treatment. Sometimes the doctor will do tests before deciding what type of treatment you need.
Some antibiotics work on many different types of bacteria, while others target only specific ones.
What side are effects associated with antibiotics?
Allergic reactions: Each year, more than 140,000 emergency department visits in America are due to antibiotic reactions alone. Nearly four out of five emergency room visits for antibiotic-related side effects are due to an allergic reaction. These reactions can range from mild rashes and itching to severe skin reactions with blisters, swelling of the face and throat, and resulting breathing problems.
Video content: side effects of antibiotics

Reducing the unnecessary use of antibiotics is the most effective way to reduce the risk of adverse effects of antibiotics. If you are already aware of your allergies, you should tell your doctor about any past reactions to medications or allergies.
C. difficile: C. difficile is a type of bacteria (germ) that causes diarrhea. If you take antibiotics, the balance of "good" bacteria that protect against infection and live in harmony with humans is destroyed in the digestive tract - antibiotics destroy the bacterial flora.
During this imbalance, you can get sick from many bacteria, including C. difficile. In addition, you can transfer bacteria into your body from contaminated surfaces or become infected with them from a healthcare environment. People taking antibiotics and receiving medical care are most at risk, especially older adults.
Antibiotic resistance: Using antibiotics can increase the risk of bacteria becoming resistant. Antibiotic-resistant infections can be severe and consequently tricky to treat - often requiring hospital treatment.
When NOT to use antibiotics?
Antibiotics are not always the right choice for every infection. For example, most sore throats, coughs, colds, flu, COVID, or acute sinusitis are viral in origin (not bacterial), so antibiotics are not needed. In addition, these viral infections are "self-limiting," meaning that your immune system usually kicks in and fights off the virus vigorously.
Video content: when should you not use antibiotics?

Incorrect and inappropriate use of antibiotics to treat viral infections can increase the risk of antibiotic resistance. Antibiotic-resistant bacteria are eventually unable to be killed entirely or effectively destroyed by the antibiotic, even though the antibiotic may have been working effectively before resistance developed. It can also reduce your chances of effective treatment in the future.
Using unnecessary antibiotics also poses a risk of side effects.
It is important not to share your antibiotic or take medicine prescribed for someone else and not to save the antibiotic to use the next time you get sick.
The most common types of antibiotics
The most common types of antibiotics are penicillins, macrolides, cephalosporins, tetracyclines, glycopeptides, and fluoroquinolones.
Video content: types of antibiotics in 7 minutes.

Penicillin is considered the first antibiotic to be developed and is still one of the most commonly used types. Macrolides are used to treat bacterial infections in the respiratory tract and gastrointestinal tract. Cephalosporins are used to treat bacterial infections in the urinary tract and brain. Fluoroquinolone is the most potent antibiotic used to treat more severe bacterial infections.
Penicillins are usually used to treat certain skin diseases, middle ear infections, and kidney and blood infections are also successfully treated.

Cephalosporins are extremely commonly prescribed to people allergic to the penicillin type of antibiotic - cephalosporins are used to treat infections such as gonorrhea, pelvic inflammatory disease, and sinusitis.

Tetracyclines treat several bacterial infections, including chest, urinary tract, pelvic, and inflammatory skin conditions. They are broad-spectrum antibiotics.

Macrolides are anti-inflammatory and immunomodulatory and can treat skin, soft tissue, respiratory, and sexually transmitted infections.

Fluoroquinolones fight infections that are often life-threatening or difficult to treat but are associated with bacterial resistance.

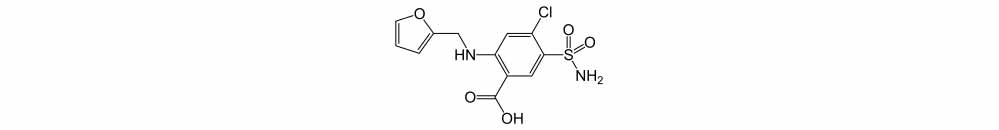
Sulfonamides - are used when the initial use of antibiotics is not successful or is contraindicated.
Glycopeptides - are used when the initial use of antibiotics is unsuccessful due to bacterial resistance. They are also used for gram-positive bacteria.

Example of a glycopeptide antibiotic: Vancomycin.
Interactions and side effects of antibiotics
Antibiotics belong to a group of drugs, and, like other drugs, antibiotics also have side effects.
To make sure that taking a particular drug is safe and without interactions, it is highly recommended, especially if you take a lot of drugs, to consult a doctor or a specialized pharmacist.
Antibiotics and alcohol
Taking medication and drinking alcohol at the same time is something you should avoid at all costs.
Antibiotics combined with alcohol, in most cases, do not cause life-threatening interactions but avoid taking alcohol and antibiotics simultaneously.
Metronidazole, in combination with alcohol, is inappropriate and should be avoided. Metronidazole is an antibiotic used for specific dental and vaginal infections.
Similar warnings apply to the antibiotic tinidazole, which is often used for the highly stubborn bacteria Helicobacter Pylori. The cessation of alcohol consumption should continue for a few days after stopping the use of the mentioned antibiotics.
Antibiotic resistance
- bacterial resistance to antibiotics is considered a huge global challenge.
- antibiotic resistance in bacteria is a fact that can happen to anyone, in the developed or underdeveloped world
- Bacterial resistance is something that happens naturally, and overprescribing antibiotics only accelerates this process
- Bacterial resistance leads to higher mortality and, among other things, longer hospital stays, higher healthcare costs, and longer hospitalizations.
Video content: what antibiotic resistance looks like (Educational)

Antibiotic resistance has become a severe and increasingly widespread problem around the world. So the excessive use of antibiotics has led to the fact that treating entirely common infectious diseases is also a problem.
In parts of the world, especially underdeveloped ones, where antibiotics can be bought without a doctor, antibiotic resistance is generally even more excellent.
The misuse and overuse of antibiotics and poor infection prevention and control accelerate antibiotic resistance. However, actions can be taken at all levels of society to reduce the use of antibiotics, especially if it is unnecessary.
What can you do yourself?
- use probiotics only when necessary and prescribed by a doctor or specialist
- never request antibiotic therapy if your doctor explains that it is not necessary in your case
- never give your antibiotics to someone else
Video content: antibiotics and bacteria - the fight against bacterial resistance.

- Act preventively - wash your hands, avoid close contact with people who have a cold or are otherwise infected, get vaccinated regularly, and prepare your diet with hygiene in mind.
- Food preparation should comply with the guidelines. - it is necessary to separate cooked food from raw and uncooked food; food must be stored at lower temperatures; use food that was raised without the use of antibiotics
What can doctors/specialists do?
- it is necessary to prevent the spread of infections by maintaining regular hygiene, hygiene of the environment in which you work, and hygiene of instruments
- prescribing antibiotics should only be done when it is necessary, by prescription guidelines
- communicate newly identified resistances to your superiors
- communicate with your patient how to take an antibiotic, how to avoid improper use, and what are the dangers of using antibiotics
- instruct the patient on how to avoid infections - examples of topics: vaccination, regular hand washing, safe sex, and protecting the mouth and nose when sneezing.
What can the agricultural sector do?
To best protect yourself against antibiotic resistance, adhere to the following tips:
- antibiotics should only be given to animals under the strict supervision of a veterinarian
- antibiotics are not intended for prevention, so they are not prescribed in such a case
Video content: what antibiotic resistance looks like in agriculture (instructive)

- antibiotics are not given to stimulate faster growth
- improve hygiene throughout the breeding process
- prevent the possibility of infection before it happens.
Latest findings
Although some new antibiotics are in development, unfortunately, none will be effective against the most dangerous forms of antibiotic-resistant bacteria.
Given the ease of travel and air travel, antibiotic resistance has become a global problem that requires the efforts of all countries and all governments.
When choosing an antibiotic, doctors also consider the following:
- Nature and severity of infection
- The state of the person's immune system (how well the drug can help fight infection)
- Possible side effects of the drug
- Possibility of allergies or other severe reactions to the drug
How to choose the right antibiotic?
Each antibiotic is effective against certain types of bacteria, and some antibiotics are broad-spectrum, meaning they work on several different types of bacteria simultaneously. When choosing an antibiotic to treat a person with an infection, doctors assess which bacteria are likely to be the cause. For example, some infections are caused by only certain types of bacteria. On the other hand, sometimes one antibiotic is predictably effective against all the bacteria most likely to be causing the infection, so further testing may not be necessary.
Image: Antibiotics are prescribed by a doctor or specialist.

Suppose infections can be caused by many different types of bacteria or bacteria that are not predictably susceptible to antibiotics. In that case, the laboratory must identify the infecting bacteria from the person's blood, urine, or tissue samples. The infected bacteria are then tested for sensitivity to different antibiotics. The results of these tests usually take a day or two and, therefore, cannot guide the initial choice of antibiotic if the infection needs to be treated immediately. In such cases, doctors usually start treatment with an antibiotic that is effective against the bacteria most likely to be causing the infection. When the test results are back, doctors change the antibiotic if necessary.
Questions and Answers
What are antibiotics used for?
Antibiotics are drugs that fight infections caused by bacteria in humans and animals by either inactivating them, making it difficult for them to grow and reproduce or allowing modification of the bacterial wall[1].
When should I take antibiotics?
Antibiotics treat ONLY certain infections caused by bacteria, such as sore throat, urinary infections, and whooping cough...
Antibiotics do NOT work on viruses, so we do not use antibiotics in such cases.
Viruses cause the following:
- cold and consequent discharge from the nose, with yellow or green discharge
- most sore throat (except strep throat)
- flu
- most cases of colds (bronchitis)[2].
What is the name of the most potent antibiotic?
Currently known worldwide as the most effective defense against disease-causing bacteria, the last line of defense has just gained a new "warrior": Vancomycin 3.0. Its predecessor is vancomycin 1.0, and until recently, it was used to fight dangerous infections, such as persistent Staphylococcus aureus[3].
Sources and references
Source: Family Health Guide. Conventional and alternative treatment, Dr. Jajo Lajovic, Publishing House Mladinska knjiga
1. Antibiotic Use Questions and Answers - https://www.cdc.gov
2. Antibiotic Do's & Don'ts - https://www.cdc.gov
3. Superantibiotic is 25,000 times more potent than its predecessor - https://www.science.org