Varicose veins are swollen and enlarged veins that usually appear in the legs and feet. They can be blue or dark purple and are often lumpy, bulging, or twisted. Symptoms are generally worse in warm weather or if you have been standing for long periods. However, they may improve when you walk around or if you rest and elevate your legs.
VARICOSE VEINS: What are VARICOSE VEINS? | Why are they created? | Risk Factors | Symptoms | Prevention | Treatment | Questions and Answers | Sources/references
Varicose veins are twisted dilated veins. Any vein close to the skin's surface (superficial) can be enlarged. Varicose veins most often affect the veins in the legs. This is mainly because standing and walking increase the pressure in the veins of the lower body - that is, in the veins of the legs.
For many people, varicose and spider veins (a mild version of varicose veins) are cosmetic concerns. In other people, varicose veins can cause unpleasant pain and extreme discomfort. From time to time, varicose veins can cause more severe problems.
What affects the formation of varicose veins?
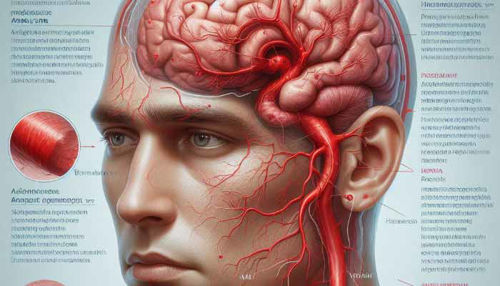
Weak or damaged valves in the veins, especially in the leg areas, can cause the formation of varicose veins. Arteries are the vessels that carry blood from the heart to the rest of the body, and veins are the vessels that return blood from the rest of the body back to the heart. To return blood to the heart, the veins in the legs must work against gravity.
Image: the display of varicose veins - these occur mainly in the leg area.

The contraction of the muscles in the lower part of the legs acts as a pump, helping the walls to return blood to the heart. Tiny valves (valves) in the veins open as blood flows toward the heart and then close to prevent blood from flowing back toward the legs. If these valves are weak or damaged, blood can flow backward and collect in the veins, causing the veins to stretch or twist.
Risk factors for the formation of varicose veins
- Age: aging causes wear and tear on the valves in the veins that help control blood flow. Over time, this wear and tear cause the valves to allow some blood to leak back into the veins, where it collects.
- Gender: women are more likely to develop varicose veins. Hormonal changes before menstruation, during pregnancy, or menopause can be a significant factor, as female hormones tend to loosen the walls of the vagina. Hormonal treatment, such as birth control pills, can also increase the risk of varicose veins.
- Pregnancy: during pregnancy, the body's blood volume increases significantly. This change supports the growing fetus, which can also affect the veins in the legs.
Video content: preventive measures against the formation of varicose and spider veins

- Family history: if other family members have had varicose veins, you are more likely to develop them too.
- Obesity: excess weight puts additional pressure on the veins.
- It prolonged standing or sitting.
Symptoms of varicose veins
Below are the most common symptoms of varicose veins. However, each individual may experience symptoms differently.
Symptoms may include:
- changes in skin color
- leg wounds
- releases
- unpleasant sensations in the legs, such as heaviness, burning, and pain
Severe varicose veins can eventually cause long-term mild swelling, leading to more serious skin and tissue problems. These include ulcers and wounds that do not heal. The symptoms of varicose veins can be similar to other medical conditions or problems. Always consult your doctor for a diagnosis.
Complications from varicose veins are rare, but it is essential to be aware of them.
Complications of varicose veins, although rare, may include:
- Ulcers: Painful ulcers can form on the skin near varicose veins, especially around the ankles. A discolored patch on the skin usually appears before an ulcer develops. See your doctor immediately if you have an ulcer on your leg.
- Blood clots: from time to time, clots form in the veins deep in the legs due to reduced blood circulation - this can cause pain and swelling of the legs, and in the worst case, the resulting clot can break off. Seek medical attention for prolonged pain or swelling in your legs, as this may indicate a blood clot is forming.
- Bleeding: occasionally, small veins on the skin may burst. Although this usually only results in local bleeding, it requires medical attention.
Talk to your GP if:
- varicose veins cause pain or discomfort
- the skin over the veins is painful and irritated
- leg pain irritates you at night and disturbs your sleep
Preventive measures can prevent the formation of varicose veins
Luckily, you can take some simple steps to improve blood flow to your legs. As a result, you can prevent the worsening of varicose veins.
1. Exercise regularly
Leg muscles are your greatest allies. Why? They help your veins push blood to your heart.
Video content: how to prevent the formation of varicose veins with Dr. Yeah?

This is very beneficial as your muscles are working against gravity. All leg exercises will also help prevent the formation of new varicose veins.
2. Maintain a healthy weight
Legs are more stressed if you are overweight. Losing extra pounds can prevent the formation of new varicose veins. In addition to helping with varicose veins, weight loss also has many benefits. It also reduces the risk of heart disease, stroke, and type 2 diabetes.
3. Avoid prolonged standing or sitting
Today's office workers are often exposed to a higher risk of developing or worsening varicose veins. So don't forget to take a break at least every half hour and get up and walk around for a while, even if it's just going to the restroom and back.
Video content: how to prevent the formation of varicose veins?

This kind of activity forces the leg muscles to move blood toward the heart more than when you are in a sitting position. So if your job requires you to stand for a long time, try to plan a break, sit down for a while, and rest - your legs will thank you.
4. Do not wear tight clothing
This can increase pressure on your legs, which can worsen varicose veins.
5. Raise your legs
Place your feet on a chair or wall so the blood can flow back toward your heart. This is especially important if you do a job requiring you to stand or sit for long periods.
6. Wear supportive compression tights.
This is also an excellent preventive measure to prevent the formation of varicose veins. Of course, these don't produce as much pressure as compression stockings, but for many, that's all they need.
Treatment and removal of varicose veins
Varicose veins usually do not require treatment. If varicose veins do not cause discomfort, you may not need to treat them. Varicose vein treatment is usually only required to relieve symptoms if your varicose veins are causing you pain or discomfort and treat complications such as leg ulcers, swelling, or skin discoloration. Some people are also treated for cosmetic reasons.
If treatment is necessary, your doctor may first recommend self-care at home.
This usually involves the following approaches:
- use of compression stockings (check blood circulation if they are suitable for you)
- regular exercise
- avoidance of prolonged state
- facilitating blood circulation - lifting the affected area during rest
If your varicose veins require further treatment or cause complications, the type of treatment will depend on your overall health and the severity of the difficulty based on the condition of your veins. A vascular specialist (doctor specializing in veins) can advise you on the most suitable treatment for you.
1. Endothermal ablation
One of the first treatments offered will usually be endothermal ablation.
Video content: endo procedure thermal ablation.

This involves using energy from high-frequency radio waves (radiofrequency ablation) or lasers (endovenous laser therapy) to seal the affected veins.
2. Radiofrequency ablation
Radiofrequency ablation involves heating the wall of a specific varicose vein using radiofrequency energy. The vein is accessed through a small incision just above or below the knee. A narrow tube called a catheter is guided into a vein under ultrasound guidance. A probe that emits radio frequency energy is inserted into the catheter.
This heats the vein until its walls collapse, closing and sealing it. Once the vein is completed, your blood will be naturally diverted to one of your healthy veins. Radiofrequency ablation can be performed under local anesthesia (you are awake) or under general anesthesia while asleep. However, the procedure may cause short-term side effects such as tingling (paresthesia). In addition, you may need to wear compression stockings for up to a week after radiofrequency ablation.
3. Endovenous laser treatment
Like radiofrequency ablation, endovenous laser treatment involves inserting a catheter into a vein and using ultrasound scanning to guide it into the correct position. Then, a small laser passes through the catheter and is positioned at the top of your varicose vein.
Video content: laser treatment procedure.

The laser emits short fragments of energy that heat the vein and close it. Then, the laser is slowly drawn along the vein using ultrasound scanning, which allows the entire vein to be completed.
Endovenous laser treatment is performed under local or general anesthesia. After the procedure, you may feel tightness in your legs, and the affected areas may be uncomfortably painful with possible bruising. Nerve damage is also potential but is usually only temporary.
4. Ultrasound-guided foam sclerotherapy
If endothermal ablation treatment is not suitable for you, you are usually offered a treatment called sclerotherapy instead. This treatment involves injecting a special foam into your veins. The foam scars the veins, closing them off.
This type of treatment may not be suitable if you have had deep vein thrombosis. The injection is administered into a vein under ultrasound guidance. It is possible to treat more than one vein in the same session.
Video content: performing the procedure: sclerotherapy with foam.

Foam sclerotherapy is usually performed under local anesthesia, where pain medication is used to numb the treated area. After sclerotherapy, your varicose veins should start to fade after just a few weeks as the more muscular veins take over the role of the damaged vein, which is no longer filled with blood.
You may need more than one treatment before the vein fades, and there is a chance that the vein will reappear and fill with blood. Although sclerotherapy is effective, it is not yet known how effective foam sclerotherapy is in the long term.
Sclerotherapy can also cause side effects, including:
- blood clots in other leg veins
- headaches
- changes in the color of the skin - for example, brown spots on the treated areas
- fainting
- temporary vision problems
You should be able to walk and return to work immediately after sclerotherapy. You will need to wear compression stockings or bandages for up to a week after the procedure. Sclerotherapy is known to have serious potential complications, such as stroke or transient ischemic attacks, in only rare cases.
5. Operation
If endothermal ablation and sclerotherapy are unsuitable treatment methods, you will usually be offered a surgical procedure called ligation and debridement to remove the affected veins.
Varicose vein surgery is usually performed with general anesthesia, meaning you will be asleep during the procedure. You can generally go home the same day, but sometimes an overnight stay in the hospital is necessary, especially if you have surgery on both legs.
6. Ligation and removal
A technique called ligation and removal involves ligation of the vein in the affected leg and then its removal. 2 small incisions are made; the first is made near your groin at the top of the varicose vein and is about 5cm in diameter. Then, a second, more minor cut is made lower down the leg, usually around the knee.
Video content: how ligation takes place - demonstration.

A thin, flexible wire is threaded through the lower part of the vein and then carefully pulled out and removed through the lower incision in your leg. The operation will not affect the blood flow in your legs; this is mainly because the veins deep in your legs will take over the role of damaged veins. However, ligation and removal may cause pain, bruising, and in some cases, bleeding.
More severe complications are rare but can include nerve damage or deep vein thrombosis, where a blood clot forms in one of the body's deep veins.
After the procedure, you may need up to 3 weeks to recover before returning to work, although this depends on your general health and the type of work you do. In addition, you may need to wear compression stockings for up to a week after surgery.
Questions and answers
What is the best way to treat varicose veins?
More prominent varicose veins are usually treated with ligation or surgical removal and laser or radiofrequency treatment. In some cases, the best combinations of the above treatments may work.
Smaller varicose and spider veins are usually treated with sclerotherapy or laser therapy[1].
How can I cure varicose veins at home?
Light exercise that improves blood flow can help reverse the unhealthy properties of varicose veins. Swimming, walking, cycling, yoga, and stretching are valuable techniques, as they provide blood circulation and exercise of the muscles without the risk of physical injury[2].
What happens if varicose veins are not treated?
If left untreated, varicose veins can develop deep vein thrombosis, a severe condition in which a blood clot forms in a deep vein. This condition is usually painful, as blood clots can break loose and become lodged in the lungs[3].
Sources and references
1. Treatment for Varicose Veins - https://stanfordhealthcare.org
2. Home Remedies for Varicose Veins - https://www.healthline.com
3. What happens if a Varicose Vein goes untreated? - https://cvvcenters.com