Nerves communicate with muscles in neuromuscular junctions. The muscle contracts when a nerve stimulates a muscle at the neuromuscular junction. Neuromuscular junction diseases include myasthenia gravis, Eaton-Lambert syndrome, and botulism.
MYASTHENIA GRAVIS: General | Symptoms of Myasthenia Gravis | Diagnosis | Treatment | Diseases of peripheral nerves | Disorders of muscle stimulation | Symptoms | Diagnosis | Treatment | Questions and Answers | Sources/references
Myasthenia gravis is an autoimmune disease in which the neuromuscular junction functions abnormally, so periods of muscle weakness occur.
In myasthenia gravis, the immune system produces antibodies that attack receptors on the muscle side of the neuromuscular junction. Those receptors that receive nerve signals through the action of acetylcholine, a chemical substance that transmits a nerve impulse through contact, are defective.
We don't know why the body attacks its acetylcholine receptors, but a genetic predisposition to this immune abnormality is essential. Antibodies circulate in the blood, and mothers with myasthenia gravis can transfer them to their unborn babies through the placenta. This transfer of antibodies causes neonatal myasthenia gravis, in which the newborn has muscle weakness that disappears within a few days to a few weeks after birth.
Symptoms
The disease occurs more often in women than in men. It usually starts between 20 and 40, although it can occur anytime. The most common symptoms are weakness of the eyelids (drooping eyelids), weakness of the eye muscles, double vision, and excessive muscle fatigue after physical activity. In about 40 percent of people with myasthenia gravis, the eye muscles are affected first; sooner or later, this problem occurs in 85 percent of patients. Difficulty speaking and swallowing and weakness of the limbs are common.
Video content: general about myasthenia gravis

It is characteristic that the muscle gradually weakens over time, so, e.g., a man who used to be able to use a hammer without difficulty becomes too weak to make repeated blows with it. The degree of muscle weakness varies from hour to hour and from day to day. The disease does not progress uniformly; exacerbations are common. In severe attacks, patients with myasthenia gravis can become completely paralyzed, but even then, they do not lose sensation.
Image: a consequence of myasthenia gravis

Approximately 10 percent of patients develop a life-threatening weakness of the muscles needed for breathing (the so-called myasthenic crisis).
Diagnosis
Doctors suspect myasthenia gravis in people with generalized weakness, especially if the weakness involves the eye or facial muscles or increases with the use of the affected muscles and improves with rest. Because acetylcholine receptors are blocked, drugs that increase the amount of acetylcholine help, so a test using one of these drugs can help confirm the diagnosis. We most often use edrophonium for the test drug; when injected intravenously, it temporarily improves muscle strength in people with myasthenia gravis. Other diagnostic tests include measuring nerve and muscle function with electromyography and blood tests for antibodies against acetylcholine.
Video content: diagnosis and symptoms of myasthenia gravis

Some people with myasthenia gravis have a thymus (thymus) tumor, which can cause the immune system to malfunction. The presence of thymoma can be demonstrated by chest imaging with computed tomography (CT).
Treatment
The disease can be treated with drugs that the patient takes, increasing the concentration of acetylcholine, e.g., pyridostigmine or neostigmine. Your doctor may increase the dose during bouts of symptoms. Patients who wake up with severe weakness or difficulty swallowing can take capsules with a longer-lasting effect in the evening. Other medications may be needed to prevent abdominal cramps and diarrhea often caused by pyridostigmine and neostigmine.
Image: treatment of myasthenia gravis with drugs.
If the dose of a drug that increases the amount of acetylcholine is too high, the drug itself can cause weakness, which is difficult for the doctor to distinguish from myasthenia. These drugs can also lose their effectiveness with long-term use, so doctors must adjust the dose accordingly. If the patient's weakness increases or the medicine is less and less effective, the situation must be evaluated by a doctor experienced in treating myasthenia gravis.
Video content: how to treat myasthenia gravis?

For people who do not respond well to pyridostigmine or neostigmine, the doctor may prescribe corticosteroids, e.g., prednisone or azathioprine. Corticosteroids may cause improvement within a few months. Current treatment regimens use corticosteroids every other day to suppress the autoimmune response. Azathioprine, a drug that helps suppress the production of antibodies, is also sometimes helpful.
We can use plasmapheresis when medicines do not relieve, or the patient has a myasthenic crisis. Plasmapheresis is an expensive procedure that removes toxic substances from the blood (in this case, abnormal antibodies). Surgical removal of the tumor helps in about 80 percent of patients with generalized myasthenia gravis.
Diseases of peripheral nerves
The peripheral nervous system includes all nerves outside the central nervous system (brain and spinal cord). The cranial nerves that connect the head and face directly to the brain, the nerves that connect the eyes and nose to the brain, and all the nerves that connect the spinal cord to the rest of the body are part of the peripheral nervous system.
The brain communicates with most of the body through 31 pairs of spinal nerves originating in the spinal cord. Each pair of spinal nerves comprises one nerve at the front of the spinal cord (carries information to the muscles) and one nerve at the back (carries sensory information to the brain). Spinal nerves are connected through plexuses in the neck, shoulders, and pelvis, and then they divide again and supply more distant body parts.
Video Content: Animation of Neuromuscular Transmission

Peripheral nerves are bundles of nerve fibers. Some are very small (measuring less than 4/10 of a millimeter in diameter), while others are large (more than 6 millimeters thick). Thicker fibers carry messages that activate muscles (motor or locomotor fibers) and sensations of touch and position (sensory or sensory fibers). Thinner sensory fibers transmit pain and temperature sensations and control automatic body functions, e.g., heart rate, blood pressure, and body temperature (autonomic nervous system). Schwann cells wrap each nerve fiber and create insulation, the myelin sheath.
Peripheral nerve dysfunction may be the result of damage to the nerve fiber itself, nerve cell body, Schwann cell, or mi--
Muscle-brain circuit
Nerves are connected and communicate their signals through synapses. Two complex nerve pathways are involved in muscle movement: a sensory pathway to the brain and a motor pathway to the muscle.
Let's take a look at the twelve fundamental steps of this process:
1. Sensory receptors in the skin detect sensations and transmit the signal to the brain.
2. The signal travels along the sensory nerve to the spinal cord.
3. The synapse in the spinal cord connects the sensory nerve to the spinal nerve. 4. The nerve passes to the opposite side of the spinal cord. 5. The signal is sent up the spinal cord. 6. A synapse in the thalamus connects the spinal cord with nerve fibers that transmit the signal to the sensory cerebral cortex. 7. The sensory cortex registers the signal and triggers the creation of a movement signal in the motor cortex. 8. The nerves that transmit the signal cross over to the opposite side at the base of the brain. 9. The signal is sent down the spinal cord.10. The synapse connects the spinal cord with the motor nerve.
11. The signal travels along the motor nerve.
12. The signal reaches the motor pad, triggering a muscle movement.

-Elin envelopes. When the myelin sheath is damaged, and the myelin disappears (demyelination), the nerves cannot transmit impulses typically. However, the myelin sheath can often regenerate quickly, allowing complete restoration of nerve function. Unlike the myelin sheath, a damaged nerve cell repairs itself and grows back very slowly, if at all. Sometimes, a cell can grow in the wrong direction, leading to abnormal nerve connections. Thus, e.g., it connects the nerve to the wrong muscle, causing jerky or awkward movements, or abnormally grows a sensory nerve so the patient feels touch or pain in the wrong place.
Disorders of muscle stimulation
The nerve signal pathway from the brain to the muscles is complex; disruptions anywhere along this pathway can cause muscle and movement problems. If the nerves do not stimulate the muscles properly, they weaken, thin out (atrophy), and can become completely paralyzed, even though they are otherwise normal. Muscle diseases originating from impaired nerve function include amyotrophic lateral sclerosis, progressive muscular atrophy, progressive bulbar palsy, primary lateral sclerosis, and progressive pseudobulbar palsy. In most cases, we do not know the cause of the disease. In about 10 percent of cases, an inherited predisposition seems to contribute to the disease's development.
These diseases are similar - all the spinal cord or brain nerves that stimulate muscle activity (motor nerves) progressively deteriorate and cause muscle weakness, which can end up as paralysis. However, each disease affects a different part of the nervous system and a different group of muscles and, thus, different body parts. These diseases are more common in men than in women. Symptoms usually start between the ages of 50 and 60.
Symptoms
Amyotrophic lateral sclerosis is a progressive disease that begins as weakness - often in the arms, less often in the legs. The weakness may progress faster on one side of the body than the other and generally spreads up the lower or upper limb. Cramps are also common and may precede weakness, but sensations remain intact. Over time, in addition to increasing weakness, spasticity appears: muscles become rigid, spasms follow, and tremors may appear. They can weaken the muscles involved in speaking and swallowing, leading to difficulty speaking (dysarthria) and swallowing (dysphagia). Sooner or later, the disease can weaken the diaphragm, causing breathing problems; some patients need a ventilator.
Amyotrophic lateral sclerosis always progresses, although the rate of progression may vary. Approximately 50 percent of patients with this disease die within three years after the appearance of the first symptoms; 10 percent of them live for ten years or more, and sometimes, a patient lives for another 30 years.
Progressive muscular atrophy is similar to amyotrophic lateral sclerosis but progresses more slowly; spasticity does not occur, and muscle weakness is less severe. The first symptoms may be involuntary contractions or twitching of muscle fibers. Many patients with this disease survive for 25 years or more.
Image: muscle atrophy
In progressive bulbar palsy, the nerves that control the muscles associated with chewing, swallowing, and speaking are affected, making these functions increasingly tricky. In patients with progressive bulbar palsy, inappropriate emotional reactions may also develop, from expressions of happiness to expressions of sadness, which pass quickly and without reason; inappropriate emotional outbursts are common. Due to difficulty swallowing, patients often inhale food or saliva into their lungs. Death usually follows 1 to 3 years after the onset of the disease, often from pneumonia.
Primary lateral sclerosis and progressive pseudobulbar palsy are rare, slowly progressive variants of amyotrophic lateral sclerosis. Primary lateral sclerosis primarily affects the upper and lower limbs, while progressive pseudobulbar paralysis affects the muscles of the face, jaw, and throat. In both diseases, muscle weakness is accompanied by severe muscle stiffness. Muscle cramps and atrophy do not develop; the disability usually progresses over several years.
Diagnosis
Doctors suspect one of these diseases is when an adult develops progressive muscle weakness without loss of sensation. Examinations and tests help rule out other causes of weakness. Electromyography, which measures the electrical activity in the muscles, can help determine whether the problems are in the nerves or the muscles.
However, laboratory tests cannot determine cats from possible nerve diseases. The doctor makes a diagnosis by considering which body parts are affected, when the disease started, which symptoms first appeared, and how the symptoms changed over time.
Treatment
We have no specific treatment for these diseases, nor know how to cure them. Physiotherapy helps the patient maintain muscle strength and prevents the muscles from tightening (contractures). People with difficulty swallowing should be fed very carefully so that food does not bump into them; some need to be fed through a tube inserted through the abdominal wall into the stomach. Baclofen is used to relieve muscle spasms. Some other medicines can also reduce muscle spasms and saliva production.
Researchers are testing some substances that promote nerve growth. So far, clinical studies have not confirmed their effectiveness.
Questions and answers
What are the three symptoms of myasthenia gravis?
Symptoms of myasthenia gravis can be as follows:
- droopy eyelids
- double vision
- problems with facial expressions
Video content: symptoms and course of myasthenia gravis disease

- chewing problems and swallowing problems
- slurred speech
- weak arms, legs, or neck
- difficulty breathing and occasionally severe breathing problems[2].
Can myasthenia gravis be cured?
There is no cure for this disease, but long-term remission is possible. You may be forced to limit some daily activities. People with only eye symptoms (ocular myasthenia gravis) may eventually develop generalized myasthenia gravis. A woman with myasthenia gravis can even become pregnant[2].
Can you live an everyday life with myasthenia gravis?
Treatment of myasthenia gravis significantly improves muscle weakness and leads a person with this medical condition to a relatively everyday life. Patients can usually participate in all daily activities, including work, and their life expectancy is almost average [3].
What is the root cause of myasthenia gravis?
In myasthenia gravis, the immune system makes antibodies that block or destroy many receptor sites in your muscles for a neurotransmitter called acetylcholine.
Image: signal transmission using neurotransmitters
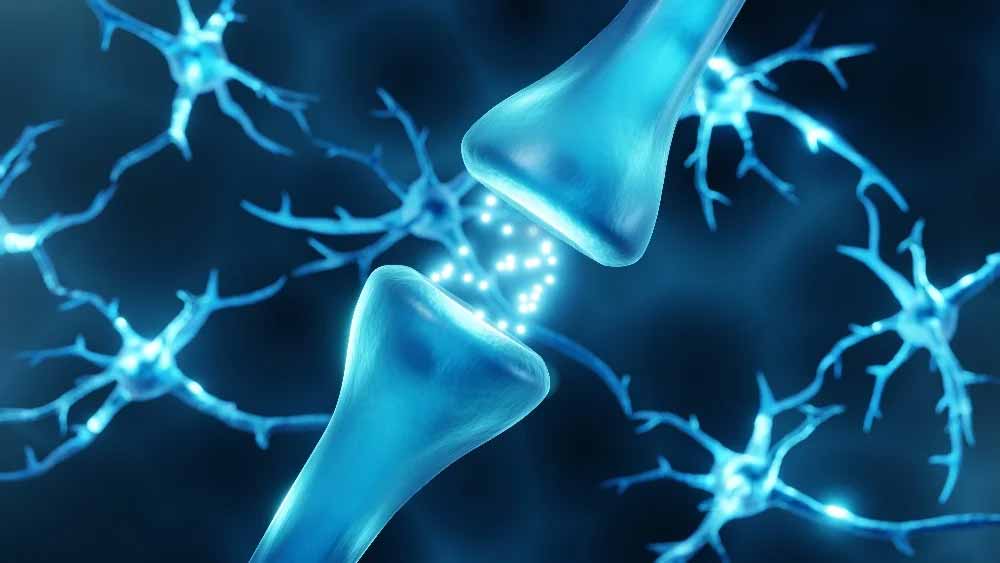
Because fewer receptor sites are available, your muscles receive fewer nerve signals. This causes weakness[4].
Sources and references
An extensive health manual for home use, Youth Book Publishing House
- Myasthenia gravis - https://www.nhs.uk
- Myasthenia gravis - https://www.mountsinai.org
- Life Expectancy of a Person With Myasthenia Gravis - https://www.medicinenet.com
- Myasthenia gravis - https://www.mayoclinic.org










 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

