Muscular dystrophies are a group of inherited muscle diseases that lead to muscle weakness (this weakness can be of varying severity). Other inherited muscle diseases include myotonic myopathies, glycogenosis, and periodic paralysis.
MUSCULAR DYSTROPHY: General | Duchenne and Becker Muscular Dystrophy | Landouzy-Dejerin muscular dystrophy | Mitochondrial myopathies | Myotonic myopathies | Glycogenoses | Periodic paralysis | Questions and Answers | Sources/references
The best-known form of muscular dystrophy is Duchenne dystrophy, which is caused by a defect in the gene for the dystrophin protein. This disease usually begins to develop in early childhood and mainly affects boys. Other notable forms include Becker dystrophy, facioscapulohumeral dystrophy, myotonic dystrophy, and limb-girdle dystrophy.
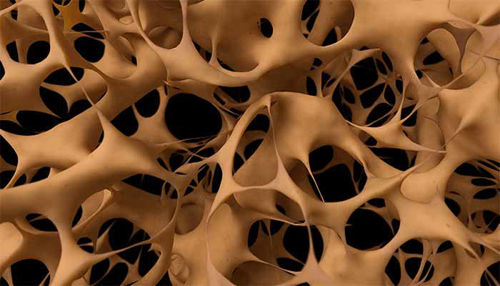
Muscular dystrophies result from mutations in genes that code for proteins necessary for the normal functioning of muscle cells. These mutations can cause damage to the structure of muscle cells, which leads to their deterioration and deterioration of muscle function.
Image: There are more than 30 types of muscular dystrophy.

Treatment of muscular dystrophies is often symptomatic, which means that it is focused on alleviating symptoms and improving patients' quality of life. This may include physiotherapy, the use of orthotics, medication to relieve symptoms, respiratory support, and nutritional therapy. However, there is currently no drug to correct the underlying genetic defect that causes muscular dystrophy. Research in gene therapy and other therapeutic options is under development.
Duchenne and Becker Muscular Dystrophy
The most common muscular dystrophies, Duchenne and Becker, are diseases that cause weakness in the muscles closest to the trunk. The gene defect that causes Duchenne muscular dystrophy differs from the one that causes Becker muscular dystrophy, and both defects are in the same gene. The gene is recessive and is transmitted on the X chromosome. A woman can carry the defective gene and not get the disease because the normal X chromosome compensates for the genetic defect on the other X chromosome. Any man who receives a defective X chromosome gets the disease.
Image: Becker muscular dystrophy occurs in 3 out of every 100,000 boys.
.jpg)
Boys with Duchenne muscular dystrophy are almost entirely without a vital muscle protein, dystrophin, which we think is essential for maintaining the structure of muscle cells. 20 to 30 out of every 100,000 newborn boys have Duchenne muscular dystrophy. In boys with Becker's muscular dystrophy, dystrophin is produced, but its molecules are too large and do not function properly.
Symptoms
Duchenne muscular dystrophy usually first appears in boys between the ages of 3 and 7 as weakness in or around the pelvis. It is usually followed by weakness in the shoulder muscles, which is constantly progressing.
Video content: Proteins for life and death - Meeting with Dr. Outflow to the rest.

When muscles weaken, they also increase in size, but the abnormal muscle tissue is not strong enough. In 90 percent of boys with Duchenne muscular dystrophy, the heart muscle also enlarges and weakens, causing problems with the heartbeat (shown on an electrocardiogram). Boys with Duchenne muscular dystrophy tend to duck, fall frequently, and have trouble walking up stairs and getting up from a sitting position. Contractures of the upper and lower limb muscles usually occur around the joints, so they cannot fully extend the elbows and knees.
Sooner or later, an abnormally curved spine (scoliosis) develops. By the age of 10 or 12, most children with this disease use a wheelchair. Due to their progressive weakness, they also become susceptible to pneumonia and other diseases, and most die before the age of 20. Although boys with Becker muscular dystrophy have similar symptoms, their disease is milder. Symptoms first appear around the age of 10. At the age of 16, only a few are confined to a wheelchair, and more than 90 percent of them are still alive at the age of 20.
Diagnosis
Doctors suspect muscular dystrophy when a little boy becomes weak, and the weakness progresses. An enzyme (creatine kinase) is leaking from the muscle cells, so the level of this enzyme in the blood is abnormally high. However, high creatine kinase activity in the blood does not necessarily mean that a person has muscular dystrophy; other muscle diseases can also cause an increased level of this enzyme in the blood.
The doctor usually confirms the diagnosis by performing a muscle biopsy, in which a small piece of muscle is removed for examination under a microscope. Under the microscope, dead tissue and abnormally large muscle fibers are usually visible in the muscle.
In the late stages of muscular dystrophy, fat and other tissues replace the dead muscle tissue. Duchenne muscular dystrophy is diagnosed when special tests show deficient concentrations of the protein dystrophin in the muscle. Among the tests that can be used to support the diagnosis are electrical studies of muscle function (electromyography) and nerve conduction.
Treatment
Although there is currently no cure to correct the underlying genetic defect, some therapeutic strategies and measures exist to manage symptoms and improve patient's quality of life.
Image: Living with a chronic illness can bring emotional challenges.
.jpg)
Corticosteroids such as prednisone or deflazacort are commonly used in treatment, especially in Duchenne dystrophy. These drugs can slow the progression of the disease, improve muscle strength, and prolong the time before problems with walking and other functions occur.
Regular physiotherapy is also an essential part of treatment. A physical therapist can recommend exercises to maintain mobility, strengthen muscles, and improve posture and balance. They can also help fit braces or aids to improve movement.
Orthopedic devices such as braces or orthoses can help support joints and prevent contractures or deformities. Patients with advanced disease may experience breathing difficulties. Using devices to support breathing, such as breathing machines or breathing therapy techniques, can help improve breathing quality and reduce the risk of complications.
Living with a chronic illness can bring emotional challenges. Whether individual or group therapy, psychological support can help patients and their families cope with these challenges. In addition to these therapeutic approaches, patients must be regularly monitored by a specialist who can monitor the progression of the disease and adjust the therapy according to the individual's needs.
Landouzy-Dejerin muscular dystrophy
Landouzy-Dejerin muscular dystrophy is inherited as an autosomal dominant gene, so a single abnormal gene causes the disease, and both males and females are affected. It usually starts between the ages of 7 and 20. The facial and shoulder muscles are always affected, so the person has difficulty lifting the upper limbs, whistling, or closing the eyelids. Some people with this disease also develop weakness in the lower part of the lower limbs, so they have difficulty bending their legs at the ankle and drooping feet.
Video content: Duchenne and Becker muscular dystrophy.

Weakness in Landouzy-Dejerin muscular dystrophy is rarely severe, and people with the disease live an everyday life. Muscular dystrophies of the shoulder or pelvic girdle cause weakness of the muscles of the pelvis (Leyden-Mobius muscular dystrophy) or shoulder girdle (Erb muscular dystrophy). These inherited diseases usually do not appear until adulthood and rarely cause severe muscle weakness.
Mitochondrial myopathies
Mitochondrial myopathies are a group of rare genetic diseases that affect muscles. They result from damage to mitochondria, the cells in the body that produce energy. Mitochondria are important for metabolism and muscle function, so defects in them can lead to a variety of symptoms, including muscle weakness, fatigue, pain, movement problems, and others.
Diagnosis
To establish a diagnosis, a sample of weakened muscle tissue must be taken with a biopsy and examined under a microscope or chemically analyzed. Because no specific treatment is available, accurate diagnosis of these rarer forms of muscular dystrophy is rarely useful.
Myotonic myopathies
Myotonic myopathies are a group of inherited diseases in which muscles cannot relax normally after contraction. This can lead to weakness, muscle spasms, and muscle shortening (contracture).
Myotonic dystrophy (Steinert's disease) is an autosomal dominant disease that affects both males and females. It causes weakness and tight, contracted muscles, especially in the hands. Droopy eyelids are also common. Symptoms, ranging from mild to severe, can appear at any age. People with the most severe form of the disease have incredibly severe muscle weakness and many other symptoms, e.g., cataracts, small testicles, premature hair loss, irregular heartbeat, diabetes, and mental retardation. They usually die by the age of 50.
Myotonia congenita (Thomsen's disease) is a rare autosomal dominant disease that occurs in both males and females. Symptoms usually begin in childhood. The hands, lower limbs, and eyelids become stiff because the muscles cannot relax.
Image: Muscular dystrophy occurs in both sexes and all ages and races.

Muscle weakness is usually minimal. The diagnosis is based on the child's characteristic appearance, the inability to quickly extend the fingers of the hand after clenching them into a fist, and the prolonged contraction of the muscle, which the doctor hits with a hammer. An electromyogram is required to confirm. The disease is treated with phenytoin, quinine, procainamide, or nifedipine to relieve muscle stiffness and spasms; however, all of these drugs have unwanted side effects. Regular exercise can also help. Patients live an every day, long life.
Glycogenosis
Glycogenosis is a group of related rare autosomal recessive hereditary diseases in which the muscles cannot metabolize sugars normally, so large stores of glycogen (a type of starch) accumulate in them. People with other forms of glycogenosis have painful cramps and weakness, usually after physical activity. These symptoms can range from mild to severe; they disappear during rest.
Pompe disease is the most severe form of glycogenosis, which usually begins in the first year of life. Glycogen accumulates in the liver, muscles, nerves, and heart, so these organs cannot function properly. We cannot cure the disease. Most children die by the age of 2. Milder forms of this disease can occur in older children and adults, who develop weakness in the upper and lower limbs and the inability to breathe deeply.
Due to muscle damage, the protein myoglobin is released into the blood. Since this is excreted in the urine, it can be measured with a urine test, which leads to a diagnosis. Myoglobin can damage the kidneys. Myoglobin concentration decreases if the patient reduces physical activity. Myoglobin in the urine can dilute large amounts of water intake, especially after physical exertion. Your doctor may prescribe diuretics to prevent kidney damage when myoglobin levels are high. Patients with glycogenosis, except for Pompe disease, are sometimes helped by liver transplantation.
Periodic paralysis
Periodic paralysis is a group of rare related autosomal dominant hereditary diseases that cause sudden attacks of weakness and paralysis. During an attack of periodic paralysis, the muscles do not respond to normal nerve impulses and may not even respond to artificial stimulation.
Video content: Challenges of diagnosis of periodic paralysis.

Seizures differ from epileptic seizures in that the patient remains fully awake and oriented. The exact form in which the disease appears varies from family to family. In some families, paralysis is associated with a high potassium concentration in the blood (hyperkalemia); in others, paralysis is associated with reduced potassium concentration (hypokalemia).
Symptoms
When the patient, who engaged in strenuous physical activity the previous day, wakes up the next morning, he may feel mild weakness in some muscle groups or the upper and lower limbs. Weakness generally lasts a day or two.
In the hyperkalemic form, attacks often begin at age ten and last 30 minutes to 4 hours. In the hypokalemic form, attacks generally occur after the age of 20 but always before the age of 30. They last longer and are heavier. Some even people with the hypokalemic form are susceptible to attacks of paralysis the day after they have consumed a lot of carbohydrates, but the attacks can also be triggered by fasting.
Diagnosis
A description of a typical attack is the most helpful to the doctor in reaching the patient's diagnosis. If possible, the doctor draws the patient's blood during the attack to determine the potassium concentration. Your doctor will also usually check your thyroid function and perform additional tests to ensure the abnormal blood potassium levels are not due to other causes.
Prevention and treatment
Acetazolamide, a medicine that changes the acidity of the blood, may prevent seizures caused by too much or too little potassium. Patients whose blood potassium concentration decreases during attacks can drink unsweetened potassium chloride solution during the attack.
Image: Muscular dystrophy usually occurs between the ages of 10 and 30.
.jpg)
Symptoms usually subside significantly within an hour. Patients with hypokalemic conditions should avoid foods containing carbohydrates and physical exertion. Patients with the hyperkalemic form can prevent attacks by frequently eating smaller meals rich in carbohydrates and poor in potassium.
Questions and answers
How many forms of muscular dystrophy do we know?
Genetic mutations cause more than 30 types of muscular dystrophy. Some types of disease are very mild and progress slowly as a person ages, causing symptoms that do not significantly affect the ability to move or perform daily activities[1].
Who most often gets muscular dystrophy?
Muscular dystrophy occurs in both sexes and all ages and races. However, the most common variant, Duchenne, usually occurs in young boys. People with a family history of muscular dystrophy are at greater risk of developing the disease or passing it on to their children[2].
Does muscular dystrophy appear at birth?
Muscular dystrophy usually appears between the ages of 10 and 30 but ranges from birth to 70 years[3]. Congenital muscular dystrophies are a group of conditions that share a common early manifestation and common muscle pathology. In the vast majority of cases of congenital muscular dystrophy, initial symptoms are present at birth or within the first few months[4].
What causes Duchenne dystrophy?
Duchenne muscular dystrophy is caused by a genetic mutation on one of the mother's X chromosomes, and researchers have identified some of the affected genes. It is caused by a genetic defect in the production of dystrophin, a protein that protects muscle fibers from degradation when exposed to enzymes[5].
Are muscular dystrophies curable?
There is currently no cure for muscular dystrophy, but various treatments can help manage the condition. Because different types can cause quite specific problems, the treatment you receive will be tailored to your needs[6].
Sources and references
Extensive health manual for home use, Youth Book Publishing House
- Types of Muscular Dystrophy - https://nyulangone.org
- Muscular dystrophy - https://www.mayoclinic.org
- What is Muscular Dystrophy? - https://www.cdc.gov
- Congenital muscular dystrophy - https://www.musculardystrophyuk.org
- Duchenne Muscular Dystrophy - https://www.hopkinsmedicine.org
- Muscular dystrophy - https://www.nhs.uk









 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

