Patients with pulmonary alveolar proteinosis often have persistent difficulty breathing but rarely die from the disease if their lungs are washed regularly. As for other treatments, e.g., with potassium iodide or enzymes that break down proteins, it is not clear how much they do. Corticosteroids are not effective, but at the same time, they increase the risk of infections.
SARCOIDOSIS: General | Symptoms | Diagnosis | Forecast | Treatment | Infiltrative lung diseases | Questions and Answers | Sources/references
Sarcoidosis is a disease in which abnormal clusters of inflammatory cells (granulomas) form in many organs. The cause of sarcoidosis is unknown. It may be due to an infection or an abnormal immune system response. Hereditary factors may be necessary.
Sarcoidosis develops mainly between the ages of 20 and 40. It is most common among Northern Europeans and American blacks. Microscopic examination of the tissue sample reveals granulomas. These granulomas may eventually disappear entirely or become scars.
Image: Sarcoidosis develops mainly between the ages of 20 and 40.
.jpg)
They often occur in the lymph nodes, lungs, liver, eyes, and skin, less often in the spleen, bones, joints, skeletal muscles, heart, and nervous system.
Symptoms
Many patients with sarcoidosis have no symptoms and are diagnosed with the disease on a chest X-ray taken for another reason. Most patients experience mild symptoms that do not progress. Severe symptoms are rare. The symptoms of sarcoidosis vary greatly depending on the location and extent of the disease. The first signs may be fever, weight loss, and mild joint pain. The lymph nodes are usually enlarged but often do not cause symptoms.
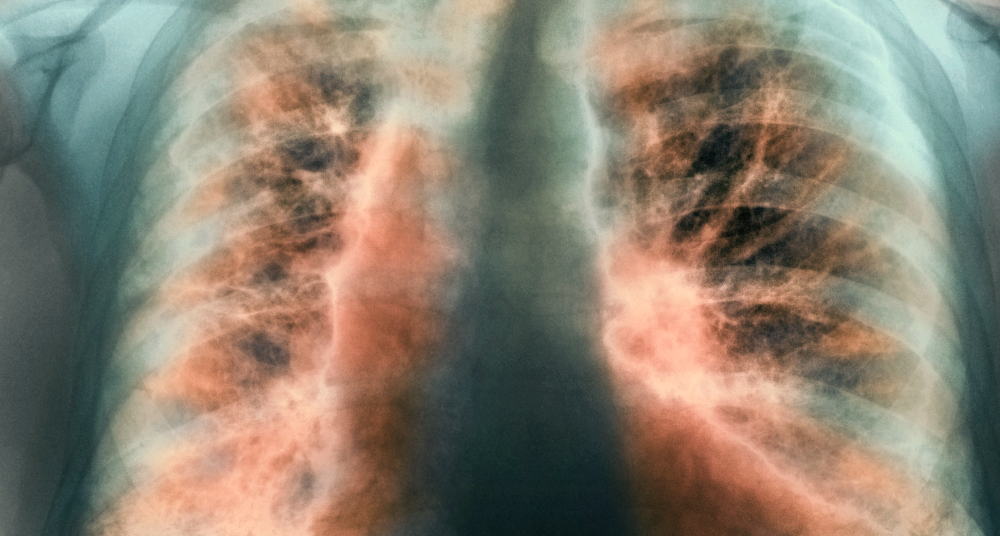
Fever can recur throughout the illness. Sarcoidosis affects the lungs the most. An X-ray may show enlarged lymph nodes where the lungs meet the heart or on the right side of the trachea. Sarcoidosis causes lung inflammation, eventually leading to scarring and cyst formation, causing coughing and shortness of breath. Severe lung damage can eventually weaken the heart.
Sarcoidosis often affects the skin. It often starts with raised, tender, red bumps, usually on the shins (erythema nodosum). They are accompanied by fever and pain in the joints. Long-term sarcoidosis can cause flat lesions (plaques), raised lesions, or lumps just under the skin. About 70 percent of patients with sarcoidosis have granulomas in the liver. They often have no symptoms, and the liver functions normally. Less than 10 percent of patients with sarcoidosis have an enlarged liver. Jaundice due to impaired liver function is rare.
Image: Sarcoidosis is often detected on a chest x-ray.
.jpg)
The eyes are affected in 15 percent of patients with sarcoidosis. Uveitis (inflammation of a particular inner part of the eye) causes the eyes to redden and hurt, and the vision is blurred. Long-term inflammation can worsen the drainage of the aqueous humor and cause glaucoma, which can lead to blindness. Granulomas can form in the conjunctiva; these often cause no symptoms, but the conjunctiva is accessible so that the doctor can take tissue samples from it for examination. Some patients with sarcoidosis complain of dry, burning, and red eyes; the cause is probably poorly functioning lacrimal glands due to the disease.
Granulomas that form in the heart can cause angina pectoris or heart failure. Those that form near the heart's electrical conduction system can trigger potentially fatal heart rhythm abnormalities. The inflammation causes widespread joint pain in some patients. The joints in the hands and feet are most often affected. Cysts form in the bones and can cause swelling and sensitivity of nearby joints.
Sarcoidosis can affect the nerves in the brain and cause double vision and laxity on one side of the face. If the pituitary gland or the bones around it are affected, diabetes insipidus develops. The pituitary gland stops secreting vasopressin, a hormone that the kidneys need to concentrate urine; this causes frequent urination and excessive urine output.
Sarcoidosis can cause calcium levels in the blood and urine to increase significantly. This happens because sarcoid granulomas create activated vitamin D, which increases calcium absorption from the gut. A high calcium concentration in the blood causes loss of running, nausea, vomiting, thirst, and excessive urine production. If the high concentration of calcium in the blood lasts for a long time, it leads to kidney stones or calcium deposits in the kidneys and, finally, kidney failure.
Diagnosis
Doctors most often recognize sarcoidosis by the characteristic X-ray shadowing. Sometimes, no further tests are needed. If they are, the diagnosis is confirmed by a microscopic examination of the tissue, which shows inflammation and granulomas.
Tuberculosis can cause similar changes to those caused by sarcoidosis, so the doctor also performs a tuberculin test to rule out the possibility of tuberculosis. Other ways to help a doctor diagnose sarcoid or assess its severity include measuring the level of angiotensin-converting enzyme (a particular enzyme) in the blood, lung lavage, and whole-body gallium scintigraphy.
Video content: Understanding sarcoidosis.

Many patients with sarcoidosis have high levels of angiotensin-converting enzymes in their blood. Lung lavages with active sarcoidosis contain many lymphocytes, but this is not specific to sarcoidosis. Gallium scintigraphy is sometimes used when the diagnosis of sarcoidosis is uncertain because it shows abnormal accumulation of tracer in the lungs or lymph nodes in patients with the disease.
In patients with scarred lungs, lung function tests show that the air the lungs can hold is less than usual. Blood tests may reveal a reduced number of white blood cells. The concentration of immunoglobulins is often high. If the disease affects the liver, there may be increased concentrations of liver enzymes, especially alkaline phosphatase.
Forecast
Sarcoidosis often gets better or goes away on its own. More than two-thirds of patients with pulmonary sarcoidosis have no symptoms after nine years. Even enlarged lymph nodes in the chest and extensive lung inflammation can disappear within months or years. More than three-quarters of those with only enlarged lymph nodes and more than half of those with lung involvement recover after five years.
Patients whose sarcoid has not spread beyond the chest do better than those with it elsewhere. Those who have enlarged lymph nodes in the chest but no signs of lung disease have an excellent prognosis. The best prognosis is for those whose disease begins with erythema nodosaur. About 50 percent of people who have previously had sarcoidosis experience a recurrence.
Image: About 50 percent of people who have previously had sarcoidosis experience a recurrence.
.jpg)
Approximately 10 percent of patients with sarcoidosis are severely affected by damage to the eyes, respiratory system, or elsewhere. Scarring of the lungs leading to respiratory failure is thought to be the most common cause of death, followed by bleeding from lung infection caused by Aspergillus fungi.
Treatment
Most patients with sarcoidosis do not need treatment. Corticosteroids control severe symptoms, e.g., difficulty breathing, joint pain, and fever. They are also prescribed if tests show a high concentration of calcium in the blood; if the heart, liver, or nervous system are affected; if sarcoidosis causes unsightly skin changes or eye involvement that is not relieved by corticosteroid eye drops; and if lung involvement worsens.
Symptomatic patients should not receive corticosteroids, although some laboratory findings may be abnormal. Although corticosteroids are good at controlling symptoms, they do not prevent scarring of the lungs over the years. About 10 percent of those who need treatment do not respond to corticosteroids and are given chlorambucil or methotrexate, which can be very effective. Hydroxychloroquine sometimes helps reverse skin changes.
Video content: Sarcoidosis - pathophysiology, diagnosis and treatment.

Treatment success can be monitored by X-rays of the chest organs, pulmonary function tests, and measurement of calcium or angiotensin-converting enzyme concentration in the blood. These tests should be repeated regularly to detect recurrences after treatment.
Infiltrative lung diseases
Several diseases with similar symptoms are caused by the enormous accumulation of inflammatory cells in the lung tissue. Early in these diseases, white blood cells and protein-rich fluid accumulate in the lung's air sacs (alveoli) and cause inflammation (alveolitis). If the inflammation persists, the fluid can harden, and the lung tissue becomes scarred (fibrosis). Extensive scarring of the tissue around the alveoli can gradually destroy the functioning alveoli and leave cysts in their place.
Idiopathic pulmonary fibrosis
Pulmonary fibrosis can be caused by many diseases, especially those that involve no. Regularity of the immune system. Despite the many possible causes, in half of patients with pulmonary fibrosis, its cause is never discovered. Such patients are said to have idiopathic pulmonary fibrosis (fibrosing alveolitis, usually interstitial pneumonia). The term idiopathic means "of unknown cause."
Symptoms and diagnosis
Symptoms depend on the extent of lung damage, the speed of disease progression, and the development of complications, e.g., infections or heart failure. The main symptoms start insidiously, like shortness of breath during exertion and reduced endurance.
Common symptoms include cough, loss of appetite, weight loss, fatigue, weakness, and undefined chest pain. Late in the course of the disease, when the oxygen concentration in the blood decreases, the skin may turn bluish, and the fingers' ends may thicken or become webbed. The strain on the heart can lead to heart failure. A heart affected to this extent by an underlying lung disease is called a pulmonary heart (or pulmonary).
Image: To confirm the diagnosis, the doctor may do a biopsy.
A chest x-ray may show scarring and cysts, but sometimes it is normal, even if symptoms are severe. Lung function tests show that the air the lungs can hold (lung capacity) is less than usual.
Blood gas analysis shows low oxygen concentration. To confirm the diagnosis, the doctor may perform a biopsy (removal of a small piece of lung tissue for examination under a microscope). He uses a bronchoscope for this. In many cases, however, a larger tissue sample must be removed through surgery.
Desquamative interstitial pneumonia, a variant of idiopathic pulmonary fibrosis, has the same symptoms, but the appearance of the lung tissue under the microscope differs. Lymphoid interstitial pneumonia, another variant, mainly affects the lower lung lobes. In about a third of cases, it occurs in patients with Sjogren's syndrome. Lymphoid interstitial pneumonia can also develop in HIV-infected children and adults. Pneumonia progresses slowly, but it can cause the formation of lung cysts and lymphoma.
Treatment and prognosis
If a chest x-ray or lung biopsy shows that the scarring is not extensive, the doctor prescribes the usual corticosteroid treatment, e.g., prednisone. The doctor assesses the patient's response to treatment with chest X-rays and lung function tests. A small number of patients who do not respond to prednisone may improve with azathioprine or cyclophosphamide.
Other treatments are directed against the symptoms: oxygen therapy to reduce the oxygen concentration, antibiotics against infections, and appropriate drugs against heart failure. In some medical centers, patients with severe idiopathic pulmonary fibrosis undergo lung transplantation. The prognosis varies widely. Most patients' condition continues to deteriorate. Some survive for many years, but a handful die within a few months.
Image: Two drugs are currently approved for treating idiopathic pulmonary fibrosis.

Desquamative interstitial pneumonia responds better to corticosteroid therapy, and patients with this variant live longer and have a lower mortality rate. Corticosteroids sometimes relieve lymphoid interstitial pneumonia.
Common causes of pulmonary fibrosis include:
- various types of organic dust (mold, bird droppings)
- irregularities of the immune system (rheumatoid arthritis, scleroderma, polymyositis, rarely systemic lupus erythematosus)
- drugs and poisons (methotrexate, busulfan, cyclophosphamide, gold, penicillamine, nitrofurantoin, sulfonamides, amiodarone, paraquat)
- infections (viral, rickettsial, mycoplasma, disseminated (miliary) tuberculosis)
- different types of mineral dust (quartz, carbon, metal dust, asbestos)
- gases, vapors, and vapors (chlorine, sulfur dioxide)
- therapeutic or industrial thermal radiation
Histiocytosis
Histiocytosis X is a group of diseases (Letterer-Sizway disease, Hand-Schuller-Christian disease, eosinophilic granuloma) in which abnormal cells of the esophagus, histiocytes, and another type of immune cells, eosinophils, proliferate. They grow significantly in the bones and lungs and often cause scarring. Letterer-Siwe disease begins before age three and is usually fatal without treatment. Histiocytes affect the lungs, skin, lymph nodes, bones, liver, and spleen. A pneumothorax (collapse of the lungs) may occur.
Video content: Histiocytosis - comprehensive review.

Hand-Schuller-Christian disease usually begins in early childhood but can also develop in late middle age. The lungs and bones are most often affected. Rarely, there is a malfunction of the pituitary gland, which causes bulging of the eyes (exophthalmos) and diabetes insipidus.
Eosinophilic granuloma usually starts between the ages of 20 and 40. It usually affects the bones and, in about 20 percent of patients, the lungs; sometimes, it affects only the lungs. If the lungs are affected, symptoms may include cough, shortness of breath, fever, and weight loss, but some patients have no symptoms. A common complication is pneumothorax (collapsed lung).
Patients with Hand-Schuller-Christian disease or eosinophilic granuloma may recover on their own. Although no therapy is beneficial, all three diseases can be treated with corticosteroids and cytotoxic drugs, e.g., cyclophosphamide. Treatment of affected bones is similar to that of bone tumors. Death is usually the result of respiratory failure or heart failure.
Idiopathic pulmonary hemosiderosis
Idiopathic pulmonary hemosiderosis is a rare, often fatal disease in which blood leaks from the capillaries into the lungs for an unknown reason. It mainly affects children, but the disease can also affect adults. Some of the blood that escapes from the capillaries is swallowed by the esophagus cells in the lungs. Blood breakdown products irritate the lungs and cause scarring. The main symptom is coughing up blood (hemoptysis).
The frequency and severity of hemoptysis depend on how often the capillaries bleed into the lungs. When the lungs become scarred, difficulty breathing occurs. Excessive blood loss leads to anemia; massive bleeding can cause death. Treatment is primarily aimed at relieving symptoms. Corticosteroids and cytotoxic drugs can help when the disease flares up. Transfusions may be necessary due to blood loss, and oxygen treatment may be necessary due to low blood oxygen concentration.
Pulmonary alveolar proteinosis
Pulmonary alveolar proteinosis is a rare disease in which the lung's air sacs (alveoli) become clogged with protein-rich fluid. The disease primarily affects people between the ages of 20 and 60 who do not otherwise have lung disease. The cause of pulmonary alveolar proteinosis is unknown. In rare cases, lung tissue becomes scarred. The disease can progress, remain unchanged, or disappear on its own.
Symptoms and diagnosis
If the alveoli are complete, the lungs cannot transfer oxygen to the blood, so most patients with this disease have difficulty breathing during exertion. Some have severe breathing problems, even when they are at rest. Most also cough but do not expectorate (unless they are smokers). A chest X-ray shows patchy shadowing of both lung wings. Pulmonary function tests show that the air the lungs can hold is abnormally small. Investigations also show a low oxygen concentration in the blood, initially only during physical exertion, later also during rest.
Image: Pulmonary alveolar proteinosis mainly affects people between 20 and 60.
.jpg)
To diagnose, the doctor takes a sample of fluid from the alveoli for examination. He used a bronchoscope to collect the sample, washed the lung segments with a saline solution, and then collected the lavage. Sometimes, during a bronchoscopy, the doctor does a biopsy (takes a sample of lung tissue for microscopic examination). Now and then, a larger tissue sample is needed, so it has to be removed through surgery.
Treatment
Patients who have no or few symptoms do not need treatment. The alveoli's protein-rich fluid can be washed out with saline during bronchoscopy for those with symptoms.
Sometimes, only a tiny part of the lung needs to be washed out, but if the symptoms are severe and the oxygen concentration in the blood is low, the patient is given general anesthesia to wash out the entire lung. Three to five days later, again under general anesthesia, another lung is washed out. One rinse is sufficient for some patients, while others need it every 6 to 12 months for many years.
Patients with pulmonary alveolar proteinosis often have persistent difficulty breathing but rarely die from the disease if their lungs are washed regularly. As for other treatments, e.g., with potassium iodide or enzymes that break down proteins, it is not clear how much they do. Corticosteroids are not effective, but at the same time, they increase the risk of infections.
Questions and answers
Can sarcoidosis be chronic?
Sarcoidosis is considered chronic in people whose disease remains active for more than 2-5 years[1].
Can sarcoidosis be fatal?
Chronic sarcoidosis is a complex disease with many comorbid conditions and can be fatal in some cases. Recognizing the causes of morbidity and mortality is essential for effective treatment selection, symptom management, and improved outcomes[2].
What are the causes of pulmonary fibrosis?
Common causes of pulmonary fibrosis include:
- various types of organic dust (mold, bird droppings)
- irregularities of the immune system (rheumatoid arthritis, scleroderma, polymyositis, rarely systemic lupus erythematosus)
- drugs and poisons (methotrexate, busulfan, cyclophosphamide, gold, penicillamine, nitrofurantoin, sulfonamides, amiodarone, paraquat)
- infections (viral, rickettsial, mycoplasma, disseminated (miliary) tuberculosis)
- different types of mineral dust (quartz, carbon, metal dust, asbestos)
- gases, vapors, and vapors (chlorine, sulfur dioxide)
- therapeutic or industrial radiation
How is the treatment of Histiocytosis diseases carried out?
Although no therapy is beneficial, all three diseases can be treated with corticosteroids and cytotoxic drugs, e.g., cyclophosphamide. The treatment of affected bones is similar to that of bone tumors.
What are the symptoms of idiopathic pulmonary fibrosis?
Symptoms depend on the extent of lung damage, the speed of disease progression, and the development of complications, e.g., infections or heart failure. The main symptoms start insidiously, like shortness of breath during exertion and reduced endurance. Common symptoms include cough, loss of running, weight loss, fatigue, weakness, and undefined chest pain.
Sources and References
An extensive health manual for home use, Youth Book Publishing House
- What is Sarcoidosis? - https://www.stopsarcoidosis.org
- Morbidity and Mortality in Sarcoidosis - https://www.ncbi.nlm.nih.gov













