Bladder infections can cause inflammation of the bladder (cystitis). Symptoms include pain and burning when urinating, increased frequency of urination, and sometimes abdominal pain. The inflammation usually improves after a course of antibiotics. There are also some steps you can take to prevent future bladder infections. Everything and more about bladder infections, bladder cancer, kidney infections and vaginal infections in this comprehensive article.
BLADDER INFLAMMATION: Symptoms of inflammation | Consult with a doctor | Causes | Diagnostics | Treatment | Conventional treatment | Alternative Treatment | Nutrition | Prevention | Questions and Answers | Sources/references
BLADDER CANCER: Cancer Symptoms | Causes of Cancer | Diagnostics | Cancer treatment | Prevention | Questions and Answers | Sources/references
BED WETTING: Symptoms | Consult with a doctor | Causes of Wetting | Healing | Conventional treatment | Alternative treatment | Managing a Wetting Problem | Questions and Answers | Sources/references
KIDNEY INFECTIONS: Symptoms of infection | Consult with a doctor | Causes of kidney infection | Diagnostics | Treatment | Conventional Treatment | Alternative treatment | Infection Prevention | Questions and Answers | Sources/references
VAGINAL PROBLEMS: Symptoms of vaginal problems | Consult with a doctor | Causes of problems | Diagnostics | Treatment | Conventional treatment | Alternative treatment | Prevention of vaginal problems | Questions and Answers | Sources/references
INFLAMMATION OF THE BLADDER
- Burning sensation when urinating. This is the most common sign of a bladder infection, although any pain or difficulty urinating can indicate an infection.
- Frequent forcing to water.
- Urine has a strong and foul smell.
- In the elderly: drowsiness, leakage of urine, mental confusion.
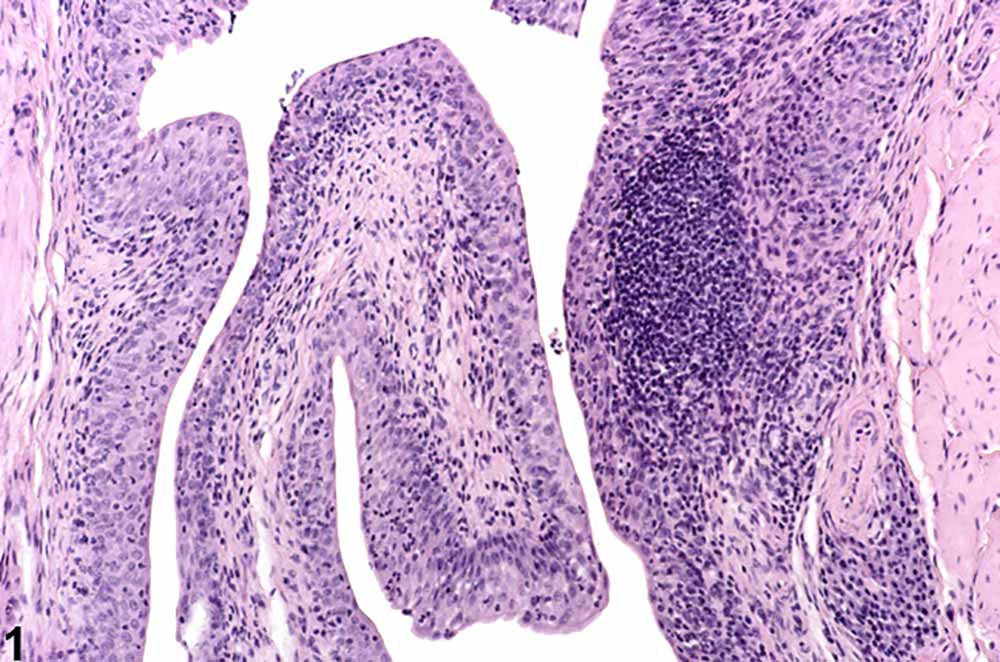
Image: cross-section of the bladder wall
In severe cases, these symptoms may be accompanied by fever and chills, abdominal pain or blood in the urine.
- Burning pain lasts longer than 24 hours after you have already tried self-medication. Untreated bladder infections can lead to more serious conditions.
- painful urination is accompanied by vomiting, fever, chills, bloody urine, abdominal or lower back pain. This could indicate possible life-threatening kidney failure, a bladder or kidney tumor, or a prostate infection. Seek medical attention immediately.
- burning pain is accompanied by discharge from the vagina or the penis, which can be a sign of a sexually transmitted disease, inflammation in small pelvis or some other severe infections. Do not delay your visit to the doctor.
- if you experience any persistent pain or difficulty urinating. It can also be a sign of an STD, vaginal infection, kidney stones, an enlarged prostate, or a bladder or prostate tumor. Do not delay your visit to the doctor.
Bladder infections are usually called cystitis, which means inflammation of the bladder. They are very common in women and quite rare in men. In fact, as many as half of women have a bladder infection at least once in their lifetime. Although doctors aren't entirely sure why women are more likely to get yeast infectionshurja than men, they suspect that this may be due to the fact that women have a shorter urethra, that is, the tube through which urine exits the bladder. This relatively short path, only about three centimeters long, makes it easier for bacteria to enter the bladder. In addition, the mouth of the urethra lies very close to the vagina and rectum, which allows bacteria from these two areas to enter the urinary tract.
Video content: symptoms of bladder inflammation

Bladder infections are generally not a serious problem if they are treated immediately. However, they can often recur, especially in susceptible people, and can lead to kidney infections, which are a more serious condition and can cause permanent kidney damage. Therefore, it is very important to treat the underlying cause of recurrent bladder infections and take appropriate preventive measures to avoid recurrent infections. Bladder infections are often difficult to diagnose in older people because the symptoms are less specific and often attributed to old age. Elderly people who suddenly become incontinent or excessively sleepy or confused should be taken to a doctor to rule out a bladder infection.
CAUSES
Most bladder infections are caused by various strains of the bacterium Escherichia coli (E. coli), which is usually found in the intestines. In women, sometimes the direct cause of a bladder infection is sexual intercourse, in which bacteria are pushed through the urethra into the bladder. Some women get an infection called "honeymoon cystitis" - almost every time they have sex. Women who use a diaphragm as a birth control method are also highly susceptible to bladder infections, probably because the diaphragm puts pressure on the bladder and prevents it from emptying completely.
Image: what bacteria in urine look like
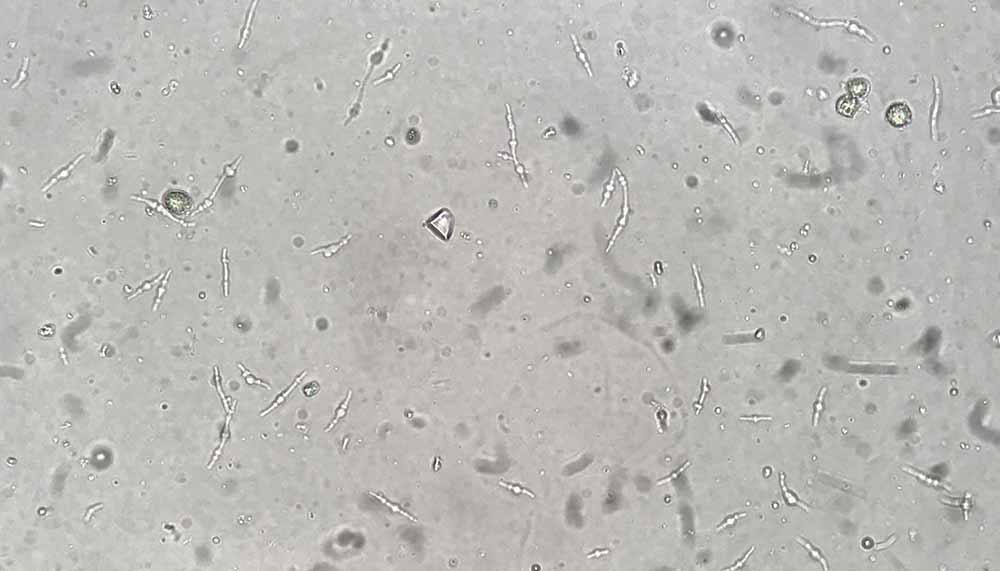
Bacteria multiply rapidly in stagnant urine in the bladder. Pregnant women whose growing fetus presses on the bladder are more susceptible to infection for the same reasons. Some people get symptoms of a bladder infection without actually having an infection. Such disorders are usually mild, but difficult to treat.
Although bladder infections can be very uncomfortable and even dangerous, when complications arise, most women heal quickly and are fairly harmless.
In men, however, a bladder infection is almost always a symptom of another disease, so it is treated with much more concern. Often the infection migrates from the prostate or some other part of the body and heralds problems in those places. But it can also mean the presence of a tumor or some other obstruction on the urinary tract. Some studies have shown that uncircumcised boys are at greater risk of bladder infection in the first year of life because bacteria can collect under the foreskin of the penis. In the past few years, an increasing number of bladder infections in both women and men have been linked to two types of sexually transmitted bacteria, chlamydia and mycoplasma. Also the use of catheters - a tube that is inserted into the bladder so that it can be emptied either at home or in hospitals - can lead to infection.
DIAGNOSTIC PROCEDURES
Bladder infections can usually be diagnosed immediately with a urine test. If you have frequent or persistent infections, or if an anatomical defect is suspected, your doctor may also recommend a cystoscopy, a diagnostic procedure in which a tube with a light is inserted through the urethra to examine the inside of the bladder. Your doctor may also want to do an intravenous pyelography (IVP) to check that your kidneys are intact. This is a special X-ray technique for examining the kidneys. The doctor may also order an ultrasound examination, which can be used to visualize all the urinary tract.
HEALING
Mild bladder infections are often cured quickly with the use of simple home remedies.
Video content: Treatment of bladder infections (cystitis), useful tips

If you do not feel any better after 24 hours, you will need to consult your doctor about treatment. If you delay cleaning the bacteria from your body, it can lead to more serious problems.
CONVENTIONAL MEDICINE
Bladder infections are treated with a range of different antibiotics to remove the infection and with pithe more fluids to flush the urinary tract. The type of antibiotic prescribed by the doctor and the determination of the number of days of taking the drug depends on the type of bacteria that caused the infection. Although some studies show that uncomplicated infections only require one to three days of treatment, your doctor may still want you to take the medication longer to get rid of the bacteria for sure. Older people and those with chronic underlying conditions such as diabetes and HIV infection will need to take antibiotics for longer, sometimes as long as 14 days.
After completing your treatment cycle, you may be required to submit a urine sample for tracking purposes. They will want to make sure that there are no signs of infection in your bladder. People with frequent bladder infections are often prescribed low daily doses of antibiotics for the next six months or longer. Patients whose infections are associated with sexual activity will be advised to take low doses of antibiotics each time they have sex. To prevent frequent recurrences of infections in postmenopausal women, some doctors prescribe the hormone estrogen as a topical ointment or in tablet form. For people whose infection is due to blockage from a kidney stone or an enlarged prostate, surgery is usually required.
ALTERNATIVE MODES
If we start treatment early, i.e. at the first sensations of burning urination, we can successfully get rid of the bladder infection with alternative methods. However, if these methods do not improve within 24 hours, you should see a doctor to prescribe an antibiotic. If you want to insist on alternative methods even while you are already taking an antibiotic in order to speed up the healing process, consult your doctor.
ACUPUNCTURE
Acupuncture treatment can help prevent recurrent bladder infections.
Image: performing acupuncture, a solution for many problems.
Consult a professional acupuncturist.
CHIROPRACTIC
Aligning the bones and joints around the pelvis can strengthen the bladder muscles and prevent recurrence of the infection. An osteopath can also provide you with this type of treatment.
HERBS
Certain herbs have been shown to be helpful both in clearing bacteria from the bladder and in relieving the burning sensation that accompanies the infection. Perhaps the most famous of all is cranberry, which recent studies have shown to have an incredible ability to fight bladder and urinary tract infections. Another herb that has been shown to be helpful in treating bladder infections is stinging nettle (Unica dioica), which has been shown to have anti-inflammatory properties. Mix 1 teaspoon of dried, crushed nettle leaves or root in one cup of boiling water. Refrigerate the infusion, then drink one soup spoon every hour or every two hours up to one cup a day.
Video content: natural herbs for the urinary tract.

The evergreen shrub uva ursi (Arctostaphylos uvaursi) or gorse, which acts as a diuretic and anti-inflammatory, has a long history as a folk remedy for bladder infections. Soak the fresh leaves in cognac or some other brandy for a few hours, then add boiling water. About one teaspoon of leaves per cup of water. If you have dried leaves, you can boil them in water without soaking them in alcohol first.
Women who have frequent infections after sexual intercourse can help prevent re-infection by rinsing the perineum with a solution of the herb hydrastea (Hydrastis canadensis) before and after intercourse. Mix 2 teaspoons of the herb in a cup of water, bring to a boil and let it simmer for 15 minutes. Cool to room temperature before use.
HOMEOPATHY
Depending on the symptoms, homeopaths recommend various remedies to ease the pain of a bladder infection. Three are most often prescribed, namely:
- if you force yourself to water and the burning sensation is very strong, cantharis,
- if you experience cramping pains when urinating or have very dark or bloody urine, mercurius corrosivus;
- for women whose infection is associated with sexual intercourse, staphysagria.
Take the medicine every hour until the symptoms disappear. If you do not feel better after 24 hours, seek medical attention.
HYDROTHERAPY AND AROMATHERAPY
Hot sitz baths help relieve symptoms of a bladder infection. If you add pungent herbal oils to the water bath, a soothing and aromatic vapor is created, which aromatherapists believe makes the treatment particularly effective. You can try adding a few drops of aromatic oils such as juniper, strawberry, eucalyptus, sandalwood, pine, parsley, cheddar, chamomile or cajeput to the bath.
CRANBERRY JUICE: A TRIED PEOPLE'S MEDICINE
For centuries Native Americans have used crushed cranberries to treat bladder infections and other urinary tract infections. Controlled studies, however, have now scientifically supported this ancient remedy. Scientific studies show that cranberries fight urinary tract infections because they contain a lot of hippuric acid, which inhibits the growth of E. coli bacteria and prevents them from sticking to the lining of the bladder.
Video content: Does cranberry juice really help with inflammatory problems of the urinary tract?

To treat an existing bladder infection and help prevent future ones, drink 3.5 to 5 dL of cranberry juice daily. However, if you prefer, you can take cranberry capsules daily, follow the instructions provided. You can also try alternating between cranberry juice and blueberry juice, which are said to have similar infection-fighting properties.
You can also try a massage oil made from 3 dag vegetable oil and 5 drops of any combination of the aforementioned herbs. Massage yourself every day and rub the oil into the area of the lower back, abdomen, stomach and hips.
NUTRITION
Both conventional and alternative healers agree that drinking plenty of fluids, urinating frequently and flushing the urinary tract well, is one of the most effective means of combating bladder infections regardless of their cause. Of course, you should avoid drinks that could irritate the bladder and worsen the burning sensation. Such culprits include alcohol, coffee, real tea, chocolate milk, carbonated drinks and citrus juices. Until the infection subsides, you should also avoid conditionally irritating foods such as citrus fruits, tomatoes, vinegar, sugar, chocolate, artificial sweeteners and very spicy foods. Once the burning sensation has subsided, wait at least 10 days before reintroducing the above drinks into your diet, one step at a time.
Supplements of vitamin C (500 mg every two hours) and vitamin A (25,000 IU daily) can help recovery. However, it is better to check with your doctor first if you are allowed to take these supplements. Vitamin C increases the acidity of urine, which inhibits the growth of bacteria, but it can affect the action of some antibiotics by making them less effective.
HOME REMEDIES
- Take acetylsalicylic acid or ibuprofen to reduce inflammation and ease the burning sensation.
- Drink cranberry juice every day.
PREVENTION
- Take care of good hygiene. After each bowel movement, carefully clean the area around the rectum. Women should wipe from front to back to avoid spreading bacteria to the urethra.
Video Content: Tips to Prevent Bladder Infections

- Empty urine as soon as you feel the need, and make sure you really empty your bladder completely.
- Wear cotton underwear and loose clothing that does not cause accumulation of heat and moisture in the perineum.
- Drink plenty of fluids.
Women:
- Empty your bladder as soon as possible after intercourse to flush out any bacteria that may have been pushed into the urethra.
- Avoid the use of scented soaps, bubble baths, scented shower gels and intimate deodorants. They contain substances that can irritate the urethra and make it more susceptible to infections.
- If you use a diaphragm to prevent pregnancy, make sure it fits well and don't leave it in your vagina for too long.
BLADDER CANCER
In its early stages, bladder cancer may not show any clear symptoms, but in its later stages, symptoms may include:
- bloody urine, which varies in color from pale brown to dark red, and sometimes contains blood clots. Traces of blood, which cannot be seen with the naked eye, are detected by examining urine samples;
- frequent urinary tract infections, pain when urinating and the need to pass water frequently;
- loss of weight orrunning;
- pain in the abdomen or lower back, constant moderately increased body temperature, anemia
CONSULT YOUR DOCTOR IF:
- you have any of the above symptoms. Although they may not be related to cancer, screening for bladder cancer is necessary.
Video content: Bladder cancer - the basics with expert John Hopkins.

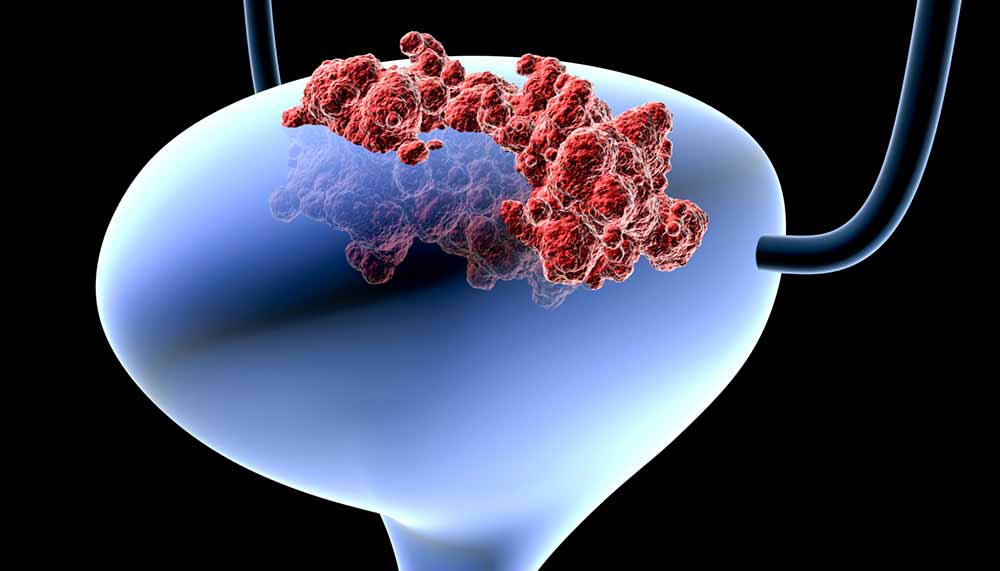
The urinary bladder is a sac in the urinary tract that stores urine after it is produced by the kidneys. The bladder is lined by specialized transitional cells, and when it is stimulated, additional layers of cells are created. Such a process creates the possibility for transitional cells to turn into cancerous ones, which then quickly help themselves and create a malignant tumor. Malignant tumors are initially small, surface lumps on the inner wall of the bladder. Cancer spreads by penetrating the muscles of the bladder and infiltrating the surrounding fat and, if left untreated, eventually invades the bloodstream and lymphatic system.
The earlier cancer is detected, the more limited it will be and the more effectively it can be treated. Thanks to better procedures for early detection, the five-year survival rate for this disease has improved from 50% in the 1960s to 70% in the 1990s. Because a bladder tumor likes to recur, early detection means it can be stopped while it's still superficial. Bladder cancer is most common after age 60; it is more common among men than among women. Approximately 150 new cases are discovered in Slovenia every year.
CAUSES
Chronic bladder irritation increases the risk of cancer. People with congenital abnormalities of the bladder, chronic bladder infections or persistent cystitis (inflammation of the bladder), as well as people with a history of a benign bladder tumor are more susceptible to it.
Video content: bladder cancer, causes, diagnosis, method of treatment

Bladder cancer itself, more than most cancers, is associated with chemical agents (carcinogens) that can cause cancer. For example, the risk of bladder cancer in smokers is three times higher than in non-smokers. This is caused by specific carcinogenic substances in tobacco smoke. Painters, truck drivers, workers in the leather industry, machinists and metallurgical workers, workers in the rubber and textile industries, and people exposed to industrial paints are more at risk. The risk is also higher in those who have already been treated with radiation or alkylating substances in chemotherapy. The consumption of nitrates in smoked and cured meats, as well as the consumption of caffeine and saccharin, may be associated with bladder cancer, although this connection is so weak that some scientists doubt it.
DIAGNOSTIC PROCEDURES
The bladder can be viewed through a fiber optic tube called a cystoscope. If the doctor finds a tumor, he will also take a small piece of tissue through this tube and send it to the laboratory for tests. If the tumor is malignant, treatment will depend on how far the cancer has spread, if at all. Blood and urine tests, X-rays of the bladder, ureters, kidneys and other organs will provide information on the size of the tumor, its localization and the extent of its spread.
HEALING
There is no other acceptable primary treatment for cancer other than that provided by an experienced oncologist.
Video content: a special way to treat bladder cancer

Alternative treatments can ease the pain caused by the disease and lessen the side effects of conventional treatment, but none have been shown to be successful in curing cancer.
CONVENTIONAL MEDICINE
If malignant formations are detected early, they can be removed by transurethral resection (TUR). In this procedure, the surgeon inserts a small tube into the bladder and either surgically removes the tumor or burns it away with heat or a laser beam. Combined with chemotherapy or radiation, TUR can also be successful in more invasive forms of bladder cancer. Immune treatment with the bacillus Calmette-Guerin (BCG) vaccine is successful in about 60% of cases. When BCG is injected into the bladder after removal of the tumor, the possibility of z is greatly reducedbut the recurrence of this tumor.
Image: presentation of bladder cancer, schematic
More invasive tumors require a more radical procedure, e.g. cystectomy or removal of the bladder. The surgeon then reroutes the urinary tract and creates an opening or stoma through which the urine flows. Patients used to have to wear external urine bags, but new techniques make it possible to make internal bags from intestinal tissue. The removal of the bladder can also mean the removal of the uterus in a woman or the prostate and testicles in a man. Although men become impotent and women infertile after this procedure, men can have prostheses implanted in their penises, while women can still be sexually active.
After surgery, radiation or chemotherapy may be needed to prevent the tumor from coming back. Anyone who has had bladder cancer should have regular checkups because cancer likes to come back. If the cancer has spread or spread beyond the bladder, surgery is usually not chosen. in the case of cancer that has reappeared, chemotherapy is the basic treatment.
ADDITIONAL MODES
Several scientific studies show that certain vitamins and minerals could be useful both in the treatment and prevention of bladder cancer. Patients receiving BCG immunotherapy may do better with mega doses of vitamins A, B6, C, and E, as well as the mineral zinc. Research also confirms that the incidence of bladder cancer is lower in people who have enough vitamin B6, beta carotene and selenium in their diet.
PREVENTION
The best thing you can do to prevent bladder cancer is to avoid all possible carcinogens. Start by not smoking. Eat smoked and dried meat only occasionally and prefer to cook fresh rather than ready-made food. If you work in an environment with carcinogenic chemicals, follow safety instructions to avoid unnecessary exposure. However, if you think that you may belong to a group that is more at risk of developing bladder cancer, make an appointment with your doctor for a regular screening program so that any cancer can be reliably detected early.
BED WETNING
SYMPTOMS
It is not unusual for children under 6 years of age to have problems with bladder control at night.
Image: bed wetting

However, you should start to worry about bed wetting if:
- is a child older than six years old and has never been dry at night or still wets the bed once or twice a month or even more often;
- your child suddenly starts wetting the bed at night after a period of being dry at night.
- efforts to teach the child how to stay dry overnight are unsuccessful or if the child wants additional help to overcome this condition.
- the child wets the bed and often passes water, or urination is painful, has dark brown urine (a sign of bleeding), abdominal pain or fever; all these symptoms can mean a urinary tract infection or a bladder infection.
- the child has side effects that may affect their behavior or disturb their sleep once they have started taking the prescribed anti-bedwetting medication. Many of the drugs prescribed for this problem can have these side effects.
The most important thing to remember about bedwetting is that it is a benign disorder and not an action with a specific purpose. Therefore, punishment is not a solution in any case. You should not worry too much about wetting the bed, unless there are children over six years old.
Video content: Bedwetting, test, alarms and treatment

Before this age, the cause may be that the child's body has not yet developed enough to be able to control the functioning of the bladder throughout the night. Time usually heals this problem; most children overcome all problems by themselves from the age of seven.
CAUSES
Why bedwetting occurs is not entirely clear, although it seems that in most cases it is a kind of developmental delay. Some experts consider it strongis simply a behavioral issue, others again think that its roots are physiological, and still others argue that both physiological and behavioral factors play a role. Only two percent of such children may have a neurological cause (usually a structural abnormality in the spinal cord), or there may be other specific causes such as diabetes or bladder infections.
Alternative practitioners believe that the cause is an improper distribution of muscles and joints around the pelvis, which can affect the sphincter muscle that controls the release of urine.
Each new stressful situation can trigger bedwetting in a child. When the child adapts to it, the problem resolves itself. But if it doesn't, the treatments listed below should definitely help. In addition, try to talk to the child about his difficulties and fears.
HEALING
CONVENTIONAL MEDICINE
To rule out problems that could be related to a disease, the pediatrician will order blood and urine tests. If these indicate that the child has diabetes or an infection, the pediatrician will treat this condition first. The doctor will also examine the child and rule out possible nerve damage.
There are three primary ways to treat bedwetting in a perfectly healthy child: waiting for the condition to go away on its own, behavioral conditioning, and drug treatment.
Waiting is the best way, but the child can feel anxious. If, however, the child is old enough to benefit from motivational counseling, to learn and become familiar with the condition and to participate in its management - he and all other family members will tolerate the disorder more easily. One form of motivation is to attach a star to the child's spreadsheet or calendar for every dry night.
Behavioral conditioning involves the use of a device with a wetness detection sensor that immediately triggers an alarm. This type of treatment has proven to be very successful. The child begins to associate a tight bladder with waking up and eventually "learns" to wake up before losing control over urination.
Medicine treatment is less successful because the condition can often recur as soon as the child stops taking the medication. However, medicines also found their place. For a short time, for example, when the child sleeps with friends, desmopressin, an antidiuretic drug, is quite effective. Doctors are increasingly avoiding the use of the antidepressant drug imipramine because of the side effects it causes.
ALTERNATIVE MODES
ACUPRESSURE
Proponents of acupressure claim that daily thumb pressure on the following points helps: Vein of conception 4, Kidney 3, Spleen 6.
Video content: acupressure therapy, which can be a very successful way to deal with the problem

You can also try holding Heart 7, the point in the hollow of your child's wrist below the little finger, for about a minute, then switch sides.
WORK WITH THE BODY
Siatsu and reflexology can be helpful for bedwetting caused by a neurological problem. Consult a trained therapist.
PHYSICAL EXERCISE
Bladder stretching exercises can help your child by increasing their bladder capacity. Once a day, from the first sign that the bladder is full, the child should hold the urine as long as possible. You and the child must then measure the amount of urine daily and determine whether the bladder volume is increasing. For this type of technique to be successful, the child must practice it for at least three months.
HOMEOPATHY
Since bedwetting is a chronic problem, you will need the help of a trained homeopath. The most common remedies are equisetum, causticum, lycopodium and pulsatilla.
MEDICINE OF SPIRIT AND BODY
Hypnotherapy can be effective in children who are highly motivated. With the help of a trained professional, the child will learn a series of working statements to repeat before going to sleep. For example: "When I have to pee, I will wake up and go to the bathroom all by myself".
NUTRITION
Sometimes bedwetting is associated with a food allergy. Try to exclude dairy products, citrus fruits and chocolate from your diet - the foods most often associated with alegia.
OSTEOPATHY
If exercises or behavioral treatments are not successful, consult an osteopath
Image: practice of osteopathy.

for manipulation of the child's low back and pelvic area, because this technique may have a beneficial effect on a possible structural problem.
WAYS TO CONTROL THE PROBLEM
- Teach an older child how to make his own bed. Put fresh pajamas and sheets in his room every night. This will help him avoid embarrassment and give him the feeling that he is in control.
- If using an alarm device for behavioral conditioning, avoid nylon pajamas and sheets. Namely, nylon can cause sweating, which triggers a false alarm.
- Prevent the mattress from getting wet and protect it with a plastic cover (which can cause the baby to sweat) or give him a small rubber blanket covered with felt to put on the wet part beds after the accident happened.
KIDNEY INFECTIONS
SYMPTOMS
- Constant pain that usually starts in the back above the waist and spreads towards the groin.
- Rapid increase in body temperature, often above 40 °C.
- Frequent need to urinate, even if the bladder is empty.
- Cloudy or bloody urine.
- Severe nausea and vomiting.
- you notice symptoms that make you think of a kidney infection; the disease is dangerous and requires immediate medical attention.
- you notice blood in your urine; it can also be a sign of kidney failure, kidney stones, a bladder or kidney tumor, a bladder infection, or a prostate infection. See a doctor without delay.
- you feel pain when you urinate or you have difficulty urinating; it can also be a sign of sexually transmitted diseases, vaginal problems, kidney stones, or a bladder or prostate tumor. See a doctor without delay.
Kidney infections occur when microbes, usually bacteria, enter the body, settle in the kidneys and cause inflammation. A kidney infection can be acute (occurring suddenly) or chronic (recurring periodically over several years). Kidney infections are dangerous.
Video content: Kidney infections, symptoms, causes and treatment.

If left untreated, they can cause permanent kidney damage and end in kidney failure. The infection can spread to the blood and cause sepsis. They can occur in all people. Pregnant women are more sensitive, partly because the fetus presses on the bladder and makes it difficult to empty it completely (the urine that remains in the bladder is a breeding ground for bacteria).
CAUSES
Like bladder infections, kidney infections are most often caused by Escherichia coli (E. coli) bacteria or other bacteria that normally inhabit the intestine. The infection usually starts in the bladder - the bacteria enter through the urethra and from there spread to the kidneys.
Infection is also caused by catheters - tubes inserted into the bladder to empty it. Catheters are inserted in patients during the recovery period after surgical procedures, sometimes also in elderly people for care in homes and in patients with neurological diseases who have impaired control over urination.
DIAGNOSTIC PROCEDURES
The doctor must examine you thoroughly and perform blood and urine tests to identify the kidney infection and determine which microbe is causing it. If you have recurrent infections or your doctor suspects that the cause of the infection is a structural abnormality, he will suggest further tests. He may order intravenous pyelography (IVP), an X-ray that shows the kidneys; cystoscopy, in which the bladder is examined with an optical tube inserted through the urethra; or an ultrasound examination that shows a detailed picture of the kidneys.
HEALING
Kidney infections require immediate treatment. If treatment is delayed and the causative agents are not removed from the body, the infection can end with serious complications.
Video content: how to cure a kidney infection?

Proponents of alternative medicine emphasize that their methods of treatment can only be used as a supplement to conventional ones.
CONVENTIONAL MEDICINE
Usually, only antibiotics and rest are necessary for an acute kidney infection to resolvestate within 48 hours. Your doctor will also tell you to drink plenty of water - at least 4 liters a day - to help your body flush bacteria from your urinary tract. Small children, the elderly and patients who have become very weak due to infection are admitted to the hospital, where they can monitor the intake of fluids and antibiotics.
Chronic kidney infections are also treated with antibiotics and large amounts of fluid. Chronic infection sometimes results from urine backing up from the bladder into the kidneys; the structural defect must be surgically repaired. Kidney infections can recur without obvious signs of illness, so your doctor will order you to have follow-up examinations and perform urine and blood tests.
ALTERNATIVE MODES
Since kidney infections are a dangerous disease, most alternative healers require you to seek conventional medical help, if you decide to supplement conventional treatment with alternative, make sure both doctors work together. Once you've cured the infection, alternative medicine can help prevent recurrences.
HOMEOPATHY
Homeopaths use "drainage remedies" or "European combinations" to help the body overcome the infection. Consult a professional experienced with these medications. One of the combinations includes apis, phosphorus and teribinthin.
NUTRITION
Until the infection is cured, avoid foods that irritate the urinary tract and put extra work on the kidneys. Irritating foods are: alcohol, coffee, salt.
PREVENTION
Most kidney infections start in the bladder, so prevention starts with preventing bacteria from entering the urinary tract.
- observe hygiene principles in the toilet. Wash thoroughly after using the toilet. Women should wipe from front to back to prevent intestinal bacteria from spreading near the urethra.
- When you feel the need, go to the toilet as soon as possible; empty the bladder completely.
- Avoid moisture and heat in the perineal area
Video content: what is the risk of kidney infection?

- wear cotton underwear and loose clothing.
- Drink plenty of fluids.
- Drink at least 3 dl of cranberry juice a day. Research has shown that cranberries contain substances that help fight urinary tract infections.
Women:
- Empty your bladder after intercourse to flush out any bacteria that have been pushed into it.
- If you use a diaphragm, make sure it fits snugly and don't leave it too long in the vagina.
- Do not use scented soaps, bubble baths and vaginal deodorants, as they all contain chemicals that irritate the urinary tract and make it more susceptible to infection.
Vaginal problems
SYMPTOMS
- The external genitalia are inflamed and itchy; you may have vulvitis.
- The skin on the external genitalia is thickened and has white patches; it could be a condition called lichen sclerosis or cancer of the external genitalia.
- Increased vaginal discharge with an unpleasant smell, burning sensation, itching and pain; you may have vaginitis.
- You have been sexually or mentally abused and experience muscle spasms and pain with every attempt to penetrate the vagina; you may have vaginismus.
- Abnormal discharge, bleeding and/or change anywhere in the vagina; it may be vaginal cancer.
- the cause of bleeding is not menstruation. If you are taking birth control pills, it may just be breakthrough bleeding, otherwise you may have dysfunctional uterine bleeding. If you are pregnant, it may be a pregnancy complication. Bleeding after menopause is sometimes a sign of uterine cancer.
- you have lower abdominal pain and fever, menstrual disorders, abnormal discharge and/or pain during intercourse. You may have an infection
in your pelvis. - you use tampons, a diaphragm, or a contraceptive sponge and get a high fever or rash. It may be toxic shock syndrome.
Video content: 13 vaginal problems presented in an interesting way.

The vagina is a part of the female genitalia that connects the cervix (entrance to the uterus) and the external genitalia - skin folds that surround the urethral and vaginal opening. This passage whichthey form flexible muscle walls, are moistened with their own secretions and from mucous glands in the cervix.
The vagina cleans itself. As secretions or discharge flow down, they wash away dead cells and other substances. The amount and quality of vaginal discharge changes with the periods of the monthly cycle, but there is almost always some. Normal vaginal discharge is clear or white.
Vaginitis is a common term that means inflammation of the vagina. Fungi cause yeast infections in the vagina, which are the most common form of infection. Other vaginal infections include bacterial vaginosis and sexually transmitted diseases, e.g. gonorrhea, trichomoniasis and chlamydia infection. All these diseases can be accompanied by itching, irritation, abnormal discharge and inflammation. Vaginal infections are very common and curable.
Bacterial vaginosis often occurs during childbearing years. For unknown reasons, the balance of vaginal bacterial flora can change so that disease-causing bacteria predominate. The main symptom is a fishy-smelling discharge, but many women with this infection have no symptoms; this also applies to infection with chlamydia and gonorrhea. For protection, you should always undergo appropriate testing during your regular gynecological examination.
Video content: Bacterial vaginosis - causes, signs, symptoms, diagnosis and treatment

Fungal overgrowth can also upset the chemical balance in the vagina. The result is a fungal infection of the vagina, which is usually characterized by itching and irritation, and a white, cheesy discharge may also appear. Fungal infections are more common in diabetics, women who take birth control pills or antibiotics, and pregnant women. However, it is estimated that around 75% of women will experience a vaginal yeast infection at some point in their lives. Many suffer from recurrent fungal infections, which are most common between the ages of 16 and 35. Vaginal yeast infections can cause pain during urination, intercourse, or both.
Vaginal infections are usually not serious. While vaginal yeast infections are primarily unpleasant, sexually transmitted diseases, e.g. gonorrhea or chlamydia infection, the associated female genitalia include the ovary, fallopian tube, uterus, cervix and vagina. The muscular, flexible walls of the vagina form the transition between the internal sex organs and the external genitalia. Various types of infections can occur in the vagina, but few are serious. However, some vaginal infections can cause complications that require medical intervention, and a greater risk of pelvic inflammatory disease and other complications. Because the external genitalia (vulva) is so close to the vagina, vulvitis often occurs with vaginitis; the infection is usually caused by the same bacteria.
Vaginal cancer, which accounts for only about 2% of all gynecological cancers, occurs mainly in women over 50 years of age. The severity of the disease depends mainly on the type of cancer and its exact localization. Two variants occur: squamous cell carcinoma and adenocarcinoma. Once vaginal cancer occurs, it can spread to surrounding tissues, including the bladder, rectum, vulva, and pubic bone.
The involuntary contraction of the lower vaginal muscles is called vaginismus. Vaginismus is a sexually related gut problem. A muscle spasm can be painful and prevent the penetration of the penis or the insertion of objects, e.g. speculum or tampon. Women with vaginismus tend to fear intercourse and associate it with pain.
CAUSES
Bacterial vaginosis is mainly caused by the dominance of Gardnerella vaginalis or Mobiluncus in the vaginal flora, but various other bacteria can also cause the disease. Stress or a new sexual partner can cause a change in vaginal flora, increasing the risk of infection.
Fungal infectionsof the vagina are caused by one of the four types of Candida fungus. Almost 80% of vaginal yeast infections are caused by an overgrowth of Candida albicans. Such an increase can be caused by a significant change in diet or the use of corticosteroids or antibiotics to treat some other disease.
Vulvitis can be caused by chemical irritation or an allergic reaction to products such as soaps or vaginal douches. Viral, bacterial or fungal infections, declining estrogen levels in menopausal women or cancer can lead to vulvitis.
Vaginism has mental causes. It most often occurs after sexual trauma, e.g. incest or rape. It can also be caused by a negative attitude towards sexuality.
During the 1950s (just as in the world from 1940 to 1970), diethylstilbestrol was prescribed to women who were at risk of miscarriage in Slovenia.(DES), a synthetic estrogen. (It was later shown not to be effective in preventing miscarriage.) Young women whose mothers took DES during pregnancy are at greater risk of adenocarcinoma.
DIAGNOSTIC PROCEDURES
Different tests are used to diagnose vulvitis. Most cases can be diagnosed with a gynecological gynecological examination, and if a sexually transmitted disease is suspected, the doctor can also order an appropriate examination or blood tests.
If vulvitis persists, a biopsy is considered as a precautionary measure to rule out malignancy.
When vaginism is suspected, the doctor will discuss with you your past sexual experiences and events, paying particular attention to mental factors.
Image: performing kegel exercises to prevent vaginismus

With a gynecological examination, he will exclude the possibility of organic changes and confirm the involuntary contraction of the muscles surrounding the vagina.
In order to diagnose vaginitis, it is necessary to determine which germ is causing the infection. They do this by examining a sample of discharge under a microscope. Once you have been diagnosed with a vaginal yeast infection, you will recognize the symptoms yourself in the future.
The diagnosis of vaginal cancer is usually based on a careful examination with a colposcope and a biopsy of suspicious-looking areas.
HEALING
The treatment of most vaginal problems, conventional or alternative, is aimed at maintaining the correct bacterial balance and alleviating irritation and discomfort.
CONVENTIONAL MEDICINE
In cases of vulvitis or bacterial vaginosis after menopause, doctors prescribe antibiotics or estrogen suppositories or topical ointment for thickening and moisturizing vaginal tissue. In other cases of bacterial vaginosis, antibiotic ointments are considered, e.g. with metronidazole or clindamycin, or metronidazole in tablets. Since the infection is often passed from one partner to another and back again, your partner may also need treatment.
Video content: Self-help for bacterial vaginosis.

If the doctor determines that the cause of the problems is a fungal infection of the vagina, he will prescribe an antimycotic, e.g. nystatin, miconazole, or clotrimazole, either in suppository or cream form. If you suffer from recurring vaginal yeast infections, over-the-counter medications are also available. These are vaginal pads, creams and suppositories that mainly contain either clotrimazole or miconazole, just like those prescribed by a doctor.
Since the causes of vaginism are mental, the best way is professional treatment for the individual and the couple.
Cancer can be a life-threatening disease. Depending on the type of vaginal cancer, your doctor will choose a combination of treatments that will be suitable for you. Local chemotherapy and laser surgery are usually recommended in the early stages. Both methods try to preserve the vagina, but this is only possible if the disease is detected early. If the tumor is extensive, the basic method is surgery. Advanced forms of vaginal cancer are usually treated with radiation. Most vaginal cancer is treated by gynecologists who specialize in the diagnosis and treatment of cancer.
ALTERNATIVE MODES
We describe additional treatments that can facilitate recovery when used in conjunction with treatments prescribed by your doctor.
HERBS
Include garlic in your diet (Allium sativum) has antibacterial, antifungal and antiviral properties and may be effective for treating vaginitis, including vaginal yeast infections. A fresh, peeled clove of garlic wrapped in gauze and inserted into the vagina can help treat bacterial vaginosis. The cartridge should be changed twice a day.
Video content: Dr. Berg about natural herbs that are important for the treatment of bacterial vaginosis

If you experience itching or mild irritation due to vaginitis, prepare a bath from an infusion of fresh common stars (Stellaria media). (Topping-
WARNING!
PRODUCTS THAT MAY BE AUCTIONED
Many women do not realize that itching and burning can be the result of irritation from products such as soaps, bath oils and crystals, spermicides, chlorine in swimming pools, feminine hygiene sprays, scented vaginal douches or moisturizing her, scented toilet paper or perfumed pads and tampons. If the doctor does not find an infection as the cause of the irritation, an allergy or sensitivity to such products is the likely culprit. Stop using the suspect product. Try cold baths in a small tub; if you want, you can add bitter salt (magnesium sulfate).
this 1 or 2 teaspoons of the plant with a cup of boiling water, let it sit for 5 minutes, then let it cool.) To reduce the inflammation associated with vulvitis and the discharge of bacterial vaginosis, an herbal vaginal wash can help. To prepare, pour 1 or 2 teaspoons of marigold (Calendula officinalis) and let it stand for 10 to 15 minutes; use the cooled tea to rinse the vagina.
HOMEOPATHY
For minor problems with the vagina, you can use the following medicines three or four times a day for a day or two.
Smelly, yellow discharge accompanied by severe burning, swelling and pain can be treated with cresotum (12c).
For itching and white or yellow discharge, sepio (12c) has been reported, and pulsatilla (12c) can help clear a thick, creamy yellow-green discharge.
If the condition does not improve, see a qualified homeopath. In some shops, homeopathic mixtures for the treatment of fungal infections of the vagina are sold over the counter.
WAY OF LIFE
If you have recurring vaginal infections, stop using tampons for six months. In addition, avoid sexual intercourse while signs of vaginal yeast infection or bacterial vaginosis are still present.
Wear cotton underpants and avoid frogs and tight clothing; this will keep the vagina cool and dry, which can help prevent vulvitis and some forms of vaginitis.
NUTRITION
If you have repeated vaginal yeast infections, get your blood sugar checked. If you are susceptible to such infections, eating yogurt with live cultures can help maintain the natural bacterial flora in the vagina.
HOME REMEDIES
Inclusion of Lactobacillus acidophilus in the diet can help eliminate vaginal yeast infections. You can make the paste from chilled capsules, which are available in some health food stores. Shake Lactobacillus acidophilus powder in the palm of your hand and add enough water to make a thick mixture, which you will apply to the vagina with a vaginal applicator or your finger.
Image: home remedies and self-help.

Regular intercourse can help prevent dryness and thinning of the vaginal walls in postmenopausal women; both increase the chance of vaginitis. The activity promotes blood circulation in the area, which keeps the vaginal tissues flexible.
Talking about inhibitions with an experienced sex therapist can help women who suffer from vaginism. Always wipe from front to back to avoid contracting germs that may be in the feces.
PREVENTION
A balanced diet always helps to maintain health. Many women are prone to vaginal infections, but some rarely have such problems. Good hygiene and consistent condom use are the best defenses against vaginitis. If you suspect that you have a vaginal infection, do not douche for 24 hours before your visit to the doctor, because otherwise you may wash away secretions that would help establish the diagnosis.
True vaginismus is the result of fear, not a physical abnormality. The best way to prevent it is a healthy home environment where sexuality is not considered dirty, but is discussed openly, honestly and realistically when appropriate. If you have survived sexual abuse or trauma, you should seek professional help.
Questions and answers
What are the symptoms of an inflamed bladder?[1]
These symptoms may include:
- Frequent urination: You may feel the need to urinate more often. Some people also experience urgency (a sudden urge to pee).
- pain/burning when urinating: During the infection, you may experience discomfort in the form of pain in the suprapubic area andburning sensation during urination.
- unpleasant smell.
How do you treat an inflamed bladder?[2]
- Use a heating pad. A heating pad placed on the lower abdomen can relieve pressure or pain in the bladder.
- Stay hydrated. Drink plenty of fluids to stay hydrated.
- Avoid coffee, alcohol, carbonated drinks with caffeine and citrus juice.
- Also avoid spicy food until the infection clears.
What causes bladder inflammation?[3]
Cystitis is inflammation of the bladder, usually caused by a bladder infection. This is a common type of urinary tract infection (UTI), especially in women, and is usually more of a nuisance than a cause for serious concern. Mild cases often improve on their own within a few days.
Sources and references
Source: Family Health Guide. Conventional and alternative treatment, Dr. Jajo Lajovic, Publishing House Mladinska knjiga
1. Bladder Inflammation (Cystitis): Bladder Inflammation (Cystitis): Causes, Symptoms & Treatment (clevelandclinic.org)
2. Cystitis: https://www.mayoclinic.org/diseases-conditions/cystitis/diagnosis-treatment/drc-20371311
3. Cystitis - https://www.nhsinform.scot/illnesses-and-conditions/kidneys-bladder-and-prostate/cystitis













