Lymphedema is a medical condition that occurs when the lymphatic system no longer functions properly, leading to fluid accumulation in the extremities and further complications. This can cause swelling in the legs, arms, and other body parts. Lymphedema often occurs after removing lymph nodes or other medical complications affecting the lymphatic system.
LYMPHEDEMA: Symptoms of lymphedema | Types of lymphedema | Consult a doctor | Causes of lymphedema | Diagnosis | Treatment | Nutrition | Treatment at home | Questions and Answers | Sources/references
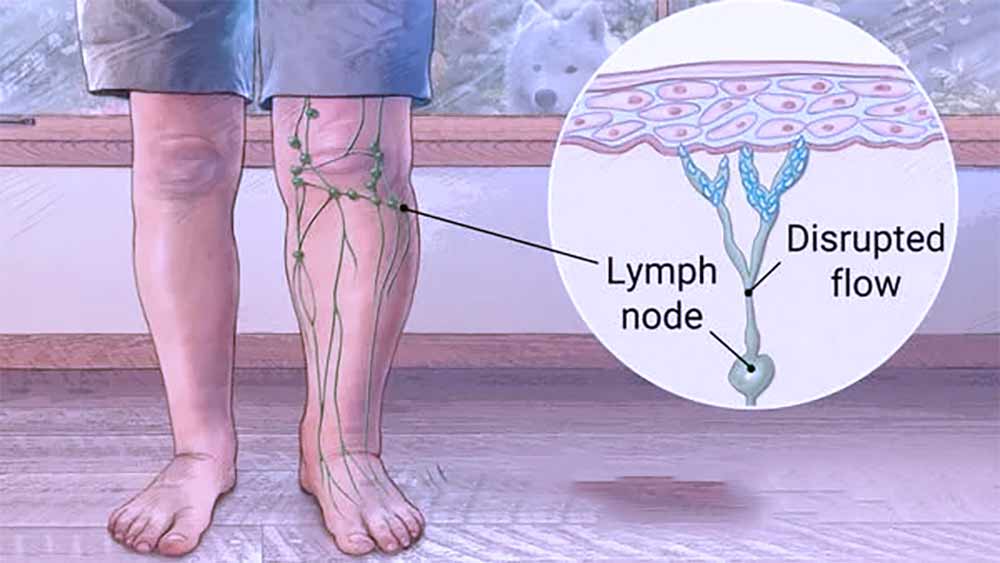
Lymphedema is swelling when the lymph vessels that make up the lymphatic system are clogged or damaged. This damage or blockage causes fluid to build up in the body's soft tissues surrounding the lymphatic vessels. The lymphatic system is part of the body's immune system and helps fight infections and protect the body from disease. It consists of a network of vessels throughout the body that carry a fluid called lymph. The lymph fluid passes through the lymphatic vessels, where it is filtered (harmful substances, bacteria, viruses, or even cancer cells). The filtered liquid is then returned to the bloodstream.
Video content: lymphedema explained

Lymphedema occurs when the lymphatic vessel system does not function properly due to a mechanical problem. As a result, the fluid cannot drain along the lymphatic vessels, so it causes swelling of the surrounding tissue. Lymphedema thus most often occurs on the arms or legs, but it can also be seen on the chest, genitals, head, and neck.
Lymph nodes are located all over the body, and their highest density is found in the neck, armpits, groin, intestines, and lung area.
Lymph fluid is a filtrate of substances harmful to the body and waste products - it also contains immune cells called lymphocytes, which destroy cancer cells and bacteria.
Symptoms of lymphedema
Lymphedema can be mild (no visible swelling), moderate (visible pitted skin), or severe (hard, oilier skin).< /p>
The main symptoms of lymphedema are as follows:
-
swelling that may come and go in the arm, leg, or other affected part of the body
-
the sensation of heaviness or pressure in the affected limb or part of the body
-
pain and discomfort in the affected limb or part of the body
-
less mobility in the affected arm or leg
-
recurrent infections of the skin
-
skin thickening
-
pitted skin (so gentle pressure on the skin leaves an indentation)
Video content: signs and symptoms of lymphedema.

Lymphedema can come and go.
Many people find that lymphedema swelling worsens:
-
it gets better during the day and then overnights
-
in the heat
-
with excessive use of the limb
-
with extended sitting or standing
-
with prolonged inactivity
If you notice any of these symptoms, you should make an appointment with a doctor.
TYPES OF LYMPHEDEMA
Primary lymphedema
Primary lymphedema is caused by changes (mutations) in the genes responsible for the development of the lymphatic system. Faulty genes cause the parts of the lymphatic system responsible for draining fluid not to develop correctly or not work as they should.
Video content: types of lymphedema

Primary lymphedema often runs in families, although not every child born to someone with the condition develops it.
Secondary lymphedema
Secondary lymphedema develops in people who previously had a regular lymphatic system that is then damaged. It can have several variations and causes.
Secondary lymphedema occurs when the lymphatic system has already been damaged and is weakened as a result, for example, due to surgery, injury, cancer therapy, or other causes. It may occur immediately after the injury or later and result from failure to treat primary lymphedema. Secondary lymphedema can also occur if the patient suffers from another disease that affects the lymphatic system, such as psoriasis, rheumatoid arthritis, or venous disease.
Picture: the cause of lymphedema - a blockage in the lymphatic duct.
Treatment for secondary lymphedema may differ from primary lymphedema and usually includes medical therapy, physical therapy, and other treatments depending on the cause of the secondary lymphedema and the degree of swelling.
Consultation with a doctor
Lymphedema is an often neglected condition that can affect your quality of life. Treatment of lymphedema can begin at the first signs, so it is essential to see a doctor immediately when you notice:
- swelling of one or both legs
- heaviness or tension in the legs
- the feeling of heaviness when walking or standing up
- difficulty wearing shoes or pants
- tingling or numbness in the legs
- inflammation or redness around the swelling
Video content: showing measurement of leg circumferences in the case of lymphedema.

If you notice any of these signs, consult your doctor, mainly so that you can start treatment and prevent the progression of lymphedema.
Causes of lymphedema
1. Cancer operation
Cancer treatment may involve invasive surgery and the removal of parts of the lymphatic system. The surgeon will try to limit damage to your lymphatic system, although this is not always possible. There is a particular risk of developing lymphedema after treatment for any cancer where the lymph glands have been removed.
Some of the most common cancers that cause lymphedema are:
-
breast cancer
-
skin cancer (melanoma)
-
gynecological cancer - such as cervical cancer and vulvar cancer
-
cancer of the genitourinary system - for example, prostate cancer or penile cancer
2. Radiotherapy
Radiotherapy uses controlled doses of high energy (radiation) to destroy cancerous tissue but can also damage healthy tissue.
Video content: how to treat lymphedema and other detailed information

Suppose radiation therapy is needed to destroy cancer cells in your lymphatic system. In that case, there is a risk that a functional lymphatic system will be permanently damaged and unable to drain fluid properly.
3. Infections
An infection such as cellulitis can sometimes cause lymphedema. Severe cellulitis can damage tissue around the lymphatic system and cause scarring.
4. Inflammation
Medical conditions that cause tissue to become red and swollen can also permanently damage the lymphatic system.
Inflammations that often cause lymphedema include:
-
rheumatoid arthritis
-
eczema
5. Venous disease
Diseases that affect blood flow through the veins can cause lymphedema in some people. Abnormal or damaged veins can cause fluid to overflow from the veins into the tissue spaces.
Image: Venous disease can be a big problem if left untreated.

This overloads and eventually exhausts the parts of the lymphatic system responsible for draining this fluid.
Some venous diseases that can cause lymphedema to include:
-
GVT (deep vein thrombosis) – a blood clot in one of the body's deep veins
-
Swollen and enlarged veins (varicose veins) - where poor blood flow in the veins causes higher pressure in the veins and more fluid to spill into the surrounding tissues
6. Obesity
Obesity is another possible cause of secondary lymphedema. People of larger build, especially very bulky ones, have an increased risk of developing lymphedema and swelling.
It is not entirely clear why this is the case, but it is thought that the extra fat tissue somehow affects the lymphatic channels and reduces the flow of fluid through them. In these cases, weight loss is an integral part of treatment, and just starting to lose weight can significantly impact swelling.
7. Trauma and injury
In many cases, lymphedema can be caused by an accidental injury to the lymphatic system. For example, it can occur after a car accident where there is extensive bruising or loss/damage to soft tissue.
8. Immobility
Movement and exercise help with lymphatic drainage because muscle activity surrounding the lymphatic vessels massages and pushes fluid into and along them. Reduced physical activity can cause lymphedema because the liquid in the lymphatic system does not move.
People with limited mobility for a long time due to various diseases, nerve damage, or arthritis may be at risk of lymphedema.
Making a diagnosis - lymphedema
If you are at risk for developing lymphedema - for example, if you have recently had cancer surgery involving your lymph nodes - your doctor can diagnose lymphedema based on your signs and symptoms.
Video content: diagnosis of lymphedema

If the cause of your lymphedema is not so obvious, your doctor may order imaging tests to check your lymphatic system.
Tests can be as follows:
-
MRI scan. MRI uses a magnetic field and radio waves to create high-resolution 3D images of the affected tissue.
-
Examination with computed tomography. This X-ray technique creates detailed cross-sectional images of body structures.
-
CT. This can reveal blockages in the lymphatic system.
-
Ultrasound. This type of test uses sound waves to create images of the internal structures of the lymphatic system. It can help find blockages in the lymphatic and vascular systems.
-
Lymphoscintigraphy. During this test, the person is injected with a radioactive dye and scanned by a machine. The resulting images show the paint moves through the lymphatic vessels and indicates blockages in the lymphatic system.
Lymphedema diagnosis
Diagnosing lymphedema can often be difficult, as it can present with very similar symptomatology to some other diseases.
In most cases, a combination of physical examination and ultrasound is used for diagnosis. In addition, information from the past and present data from the patient's medical record are often beneficial.
In some cases, performing a tissue biopsy or a CT scan makes sense. Based on all this information and symptoms, the doctor will determine whether the cause of the increased swelling is lymphedema or some other disease.
Treatment
There is no cure for lymphedema.
Image: the appearance of lymphedema in the leg area.
Treatment is aimed at reducing swelling and preventing further complications.
Medicines
Lymphedema dramatically increases the risk of skin infections (cellulitis). Your doctor may prescribe antibiotics to keep on hand so you can start taking them as soon as symptoms appear.
Therapy
Specialist lymphedema therapists can teach you about techniques and equipment that can help reduce further lymphedema swelling:
-
Exercises. A gentle contraction of the muscles in the arm or leg usually helps to remove excess fluid from the swollen limb.
-
Manual lymphatic drainage. Therapists trained in this massage-like technique use very light pressure to move trapped fluid in a swollen limb toward an area with functioning lymphatic vessels. People should avoid manual lymphatic drainage if they have a skin infection, blood clots, or active cancer in the affected limb.
-
Compression bandages. Low-stretch bandages to wrap the entire limb encourage lymph fluid to flow back toward the trunk.
-
Compression clothing. Tight-fitting elastic sleeves or not gauze can compress the arm or leg and thus stimulate the outflow of lymph fluid from the problem area. These garments often require a prescription to ensure the proper amount of compression. In addition, you may need to be measured by a professional to ensure an appropriate fit.
-
Sequential pneumatic compression. A sleeve worn over the affected arm or leg is connected to a pump that periodically inflates the sleeve, putting pressure on the limb and moving lymph fluid away from the fingers or toes.
Surgical and other interventions
Surgical treatment for lymphedema may include:
-
Lymph node transplant. Lymph nodes are taken from another part of the body and then attached to the network of lymphatic vessels in the affected limb. Many people with early-stage lymphedema see good results from this surgery, and it can reduce the amount of compression needed.
-
New drainage routes. Another option for early-stage lymphedema relief, this procedure creates new connections between the lymphatic network and blood vessels. Excess lymph fluid is then removed from the limb via the blood vessels.
-
Removal of fibrous tissue. In severe lymphedema, the soft tissues in the limb become fibrous and stiff. Removal of this hardened tissue, often in conjunction with liposuction, can improve limb function. In addition, hardened tissue and skin can be removed with a scalpel in very severe cases.
Nutrition during lymphedema treatment
The menu for lymphedema must be varied, but at the same time, contain certain nutrients that can help treat and prevent lymphedema. Therefore, you should include lots of fresh vegetables and fruit in your menu, which are rich in vitamins, minerals, and antioxidants.
Video content: diet in case of lymphedema.

Proteins such as meat, fish, eggs, legumes, and nuts should also be present in the diet, as they are necessary for building and repairing tissues. In addition, it would be best to drink enough fluids to prevent constipation and water retention. In the case of lymphedema, it is also important to avoid sugar and unhealthy fats, as they can negatively affect the functioning of the lymphatic system.
A concrete example of a menu:
- Breakfast: oatmeal with fruit and milk or yogurt, a cup of green tea
- Snack: some nuts or seeds, a cup of green tea
- Lunch: roasted vegetables (carrots, zucchini, tomatoes) with spinach and tofu, whole grain bread with butter or hummus
- Snack: an apple or other fresh fruit, a cup of green tea
- Dinner: soup with vegetables and white beans, rice with boiled beans and vegetables, a cup of green tea
- Before bed: a cup of milk or unsweetened almond milk.
All meals should contain fresh vegetables and whole grain, semi-white bread. Healthy fats such as nuts, seeds, and butter should also be included in the menu. Drinking plenty of fluids, especially green tea, is also essential, which helps strengthen blood vessel walls. In the case of lymphedema, following a healthy, balanced diet is necessary, as being overweight can contribute to an increased risk of lymphedema.
Lymphedema treatment at home
Treatment of lymphedema at home is possible, but only after careful prior instructions from a physician or therapist.
- Perform muscle-strengthening exercises regularly to prevent lymphedema from developing or worsening.
- Use compression socks or pants to reduce swelling.
- Avoid prolonged standing in one place, sitting, or lying down to prevent stagnation of lymphatic fluid.
- Limit your salt intake to prevent excessive swelling.
- Clean your skin and wounds regularly to prevent infections.
- Consult with a physical therapist or doctor from time to time for help with the effective use of compression devices and exercises.
Questions and answers
What is lymphedema?
Lymphedema is a chronic disease that often occurs due to disorders in the lymphatic system. It can appear in the extremities: arms, legs, abdomen, and chest.
Why does lymphedema occur?
Lymphedema can occur due to injury or possible removal of lymph nodes from speaking for the flow of lymph. It can also occur due to chronic infection, disease, or after radiotherapy.
How is lymphedema treated?
Lymphedema can be treated primarily with massages performed by a professional masseur, compression stockings, and medications. In some cases, surgical treatment can also be used.
Can I prevent lymphedema?
Lymphedema can, in some cases, be prevented by timely treatment of the disease that causes it and by timely detection and treatment of damage to the lymph nodes.
Can I cure lymphedema?
Lymphedema can be treated and subsequently reduced, but it is usually not completely cured. Therefore, treatment and preventive measures must be carried out all the time to prevent the condition from worsening.
How can I improve the quality of my life with lymphedema?
- Regular physical exercises can keep your muscles in good condition and improve blood circulation.
- Use elastic or compression socks.
- Do not overeat salt, as this can cause swelling.
- Drink plenty of fluids and avoid alcohol, as it can cause swelling.
- Get regular massages and physiotherapy to improve blood circulation and reduce swelling.
What can I do if I have lymphedema?
Lymphedema can be a huge hindrance in your daily life, but there are some things you can do to improve your quality of life:
- Wear appropriate, comfortable, and supportive underwear to reduce the risk of swelling and facilitate lymph drainage.
- Perform physiotherapy or massage problem areas regularly.
- Lead a healthy lifestyle, including a healthy diet and regular exercise, to improve blood circulation and speed up wound healing.
- Use compression stockings or other compression devices to help maintain good circulation.
- Consult your doctor about the possibility of using medications to help reduce lymphedema symptoms.
- Seek support from a lymphedema group or talk to a therapist to learn techniques for dealing with lymphedema.
What happens if lymphedema is not treated?
Its main symptom is swelling of the hands or feet but left untreated; lymphedema can cause severe discomfort and life-threatening infections. The swelling associated with this disease is caused by damage to the lymphatic system, a lesser-known part of the body's circulatory system[1].
Is lymphedema a severe condition?
It is essential to know that lymphedema can sometimes become severe, cause serious problems, and is often a long-term or chronic condition. Therefore, early and careful treatment is necessary to reduce symptoms and prevent worsening[2].
What is the life expectancy due to lymphedema?
When untreated lymphedema is prolonged, it can develop into lymphangiosarcoma, lymph-related cancer that limits a patient's life expectancy from a few months to two years[3].
>
Sources and references
1. https://www.cdc.gov - Lymphedema
2. Advances and challenges in treating lymphedema - https://www.nhlbi.nih.gov
3. What Is Lymphedema? - https://www.cancer.org











 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

