Vasculitis is inflammation of blood vessels. It is not an independent disease but a process accompanying many autoimmune connective tissue diseases, such as rheumatoid arthritis and systemic lupus erythematosus. Vasculitis can also occur independently without the involvement of connective tissue.
VASCULITIS: General | Polychondritis | Polyarteritis nodosa | Polymyalgia rheumatica | Temporal arteritis | Questions and Answers | Sources/references
In most patients, the triggering factor is unknown, but in some, hepatitis viruses are involved. Inflammation is thought to begin when the immune system mistakenly recognizes healthy tissue as foreign tissue and attacks it. Inflammatory cells of the immune system surround and infiltrate the affected vessels, thus destroying them and, at the same time, destroying the tissue they supply. The veins become abnormally permeable or become blocked.
In both cases, blood flow to nerves, organs, and other body parts is impaired. Areas with impaired blood circulation (ischemic areas) may be permanently damaged. The symptoms result from direct damage to the vessels or damage to the tissues supplied by these vessels.
Picture: Most forms of vasculitis are chronic.
.jpg)
All veins can be affected. Vasculitis can be limited to veins, large or small arteries or capillaries, or vessels in a specific body part, e.g., the head, leg, or kidney. Diseases such as Henoch-Schonlein syndrome, erythema nodosum, polyarteritis nodosa, temporal arteritis, and Takayasu's arteritis are characterized by vasculitis limited to vessels of a specific size or depth.
Diseases characterized by vasculitis:
| Disease | Description |
| Henoch-Schonlein purpura | Inflammation of small veins that appear as complicated, purple nodules in the skin. |
| Erythema nodosa | Inflammation of the blood vessels in the deep layer of the skin, which shows up as tender, red bumps under the skin on the hands and feet. |
| Polyarteritis nodosa | Inflammation of medium-sized arteries and impaired blood circulation through and in the surrounding tissue. |
| Temporal arteritis | Inflammation of the arteries in the brain and head, sometimes causing headaches and blindness. |
| Takayasu arteritis | Inflammation of large arteries, such as the aorta and its branches, causes their blockage and loss of pulse. |
Polychondritis
Recurrent polychondritis is a rare disease characterized by periods of destructive, painful inflammation of the cartilage and other connective tissue in the ears, joints, nose, throat, trachea, trachea (bronchi), eyes, heart valves, kidneys, and blood vessels. The disease affects men and women equally, usually in middle age.
Symptoms
Typically, both ears become red, swollen, and very painful. At the same time or later, arthritis occurs, which is either mild or severe. Any joint can be affected. Inflammation of the cartilage that connects the ribs to the sternum can develop. Inflammation of the nasal cartilage is also joint. Inflammation can also develop in the eyes, throat, trachea, inner ear, heart, blood vessels, kidneys, and skin.
Video content: Vasculitis: Everything you need to know.

Starts of inflammation and pain last a few weeks, then disappear and recur for years. The result is damage to the supporting cartilage, the ears soften and sag, the nose becomes saddle-shaped, and the patient may suffer from vision, hearing, and balance problems. Patients with this disease can die if the airways collapse or if the heart or blood vessels are severely damaged.
Diagnosis and treatment
A doctor makes a diagnosis of recurrent polychondritis when he observes the development of at least three of the listed symptoms: inflammation of both ears, pain and swelling in many joints, inflammation of the nasal cartilage, inflammation of the eye, cartilage defects in the respiratory tract, and hearing or balance defects. A biopsy of the affected cartilage reveals characteristic defects and laboratory blood tests reveal signs of chronic inflammation.
Mild recurrent polychondritis is treated with acetylsalicylic acid (Aspirin) and other non-steroidal anti-inflammatory drugs, e.g., ibuprofen. In the more severe form, the patient receives daily doses of prednisone; when symptoms improve, it should be discontinued quickly. Critically ill patients are sometimes given immunosuppressive drugs, e.g., cyclophosphamide. Although these drugs improve the symptoms of the disease, it has not been proven that they would change the course of the disease.
Nodular polyarteritis
Polyarteritis nodosa is a disease in which inflammation develops in medium-sized arteries, reducing blood flow to the organs they supply. The disease is often fatal if not properly treated. It usually appears around 40 or 50 but can occur at any age. Men are three times more likely to develop this disease than women.
Image: Men are three times more likely to develop this disease than women.
.jpg)
Its cause is unknown; it can occur as a reaction to certain drugs or vaccines. A viral or bacterial infection sometimes triggers inflammation, but no trigger event or substance can most often be found.
Symptoms
The disease may be mild at first but can end in death within a few months, but sometimes, it develops barely noticeably as a chronic disease with severe impairments. Any organ or a combination of several organs can be affected; symptoms depend on the affected organs. Often, the disease picture is similar to other diseases in which inflammation of the arteries (vasculitis) occurs.
The most common early symptom is fever. Abdominal pain, numbness and tingling in the hands and feet, weakness, and weight loss may also occur early. Three-quarters of patients develop kidney failure; they have high blood pressure and swelling due to water retention in the body and produce very little or no urine.
Suppose the blood vessels in the gastrointestinal tract are affected. In that case, a part of the intestine may be perforated, and an infection in the abdominal cavity (peritonitis) may develop, accompanied by severe pain, bloody diarrhea, and high fever.
Video content: Polyarteritis nodosa and Kawasaki disease.

Damage to the heart's blood vessels can cause chest pain and heart attacks. Damage to the brain's blood vessels can cause headaches, convulsions, and hallucinations. Liver damage can be severe. Muscle and joint pains are common, and joints can be inflamed. There are palpable bumps in the blood vessels under the skin, and skin ulcers can develop above them.
Diagnosis and treatment
Polyarteritis nodosa cannot be confirmed by blood tests alone. The doctor suspects him due to a combination of symptoms and laboratory findings that he cannot explain otherwise. Polyarteritis nodosa is also suspected when a previously healthy middle-aged man develops fever and neurological signs such as areas of numbness, tingling, and paralysis.
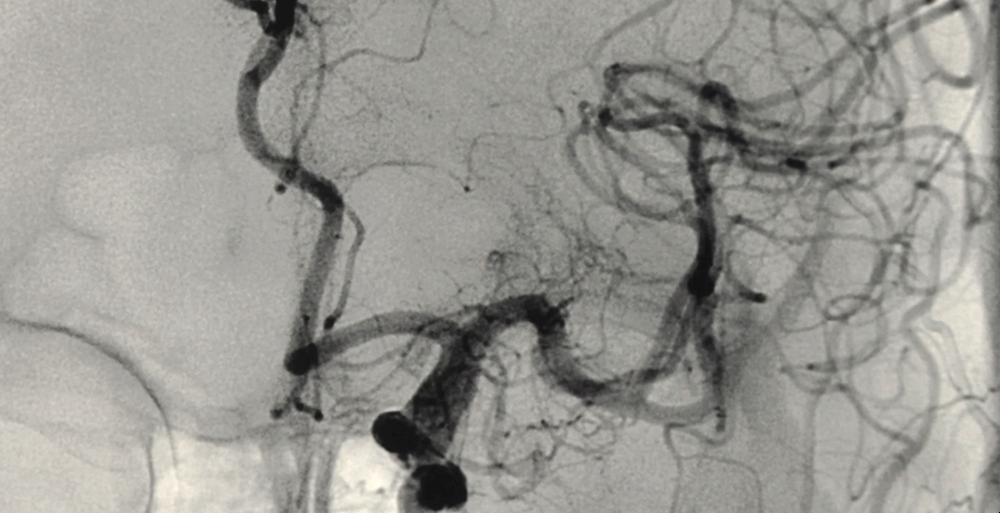
The diagnosis is confirmed with a biopsy of the affected blood vessel. Sometimes, a liver or kidney biopsy is also needed. Arteriography can detect vascular defects. Only 33 percent of patients survive one year without treatment, and 88 percent of them die within five years. Death can be prevented with aggressive treatment.
The patient must stop taking all medications that could trigger the disease. High doses of corticosteroids, e.g., prednisone, are used to try to prevent the worsening of the disease. One-third of the patients achieve an improvement and a period without disease symptoms. Corticosteroid treatment is usually long-term, so the dose is reduced when the symptoms improve.
Image: Arteriography can detect vascular defects.
If corticosteroids do not reduce the inflammation sufficiently, they are replaced, or drugs that inhibit the immune system (immunosuppressive drugs) are added to them, e.g., cyclophosphamide. Other forms of treatment are usually also needed, e.g., lowering blood pressure that is too high to prevent damage to internal organs.
Despite treatment, vital organs can fail, or weakened blood vessels can rupture. A common cause of death is kidney failure. Life-threatening infections can occur because prolonged exposure to corticosteroids or immunosuppressants can weaken the body's natural defenses against infections.
Polymyalgia rheumatica
Polymyalgia rheumatica is a disease characterized by severe pain and stiffness in the neck, shoulders, and hip muscles. It occurs in people over 50 and is twice as common in women as in men. The cause is unknown. Although severe pain is present, it does not cause muscle weakness or damage. Sometimes, it occurs together with temporal (gigantocellular) arteritis.
Symptoms
Polymyalgia rheumatic causes severe pain and stiffness in the neck, shoulders, and hips. Stiffness is worse in the morning and after periods of rest. Muscular symptoms are accompanied by fever, uncharacteristic discomfort, weight loss, and depression. All these symptoms can appear either suddenly or gradually.
Diagnosis and treatment
The doctor makes a diagnosis based on the examination and test results. A muscle tissue biopsy is usually unnecessary, but it shows no signs of muscle damage if it is done. Electromyography also shows no abnormalities. Blood tests reveal anemia. The only blood test that is usually abnormal is the erythrocyte sedimentation rate, which is significantly elevated. The muscle enzyme creatine kinase concentration in the blood, which is increased in polymyositis, is expected in polymyalgia rheumatica.
Video content: Polymyalgia Rheumatica: A Visual Explanation for Students.

Polymyalgia rheumatica usually improves dramatically with even low doses of the corticosteroid prednisone. When temporal arteritis is also present, higher doses of corticosteroids are required. The dose should be gradually reduced to the minimum effective interval when symptoms improve.
Most patients can stop taking corticosteroids after 2 to 4 years, but some need low doses for more extended. Acetylsalicylic acid and other NSAIDs may achieve less complete improvement.
Temporal arteritis
Temporal (gigantocellular) arteritis is a chronic inflammatory disease of the large arteries. The disease affects about 1 in 1,000 people over the age of 50, slightly more women than men. Its cause is unknown. Symptoms overlap with those of polymyalgia rheumatica; maybe they are just variants of the same disease.
Symptoms
Symptoms can be different depending on which arteries are affected. Usually, the large arteries in the head are affected. A severe headache suddenly appears in the shadows or the back of the head. The veins in the shadows are swollen and wrinkled to the touch. While combing the hair, the scalp is sensitive. Double or blurred vision, significant vision loss, blindness in one eye, or other vision problems may occur.
Image: Temporal arteritis causes blindness in 20% of untreated patients.
.jpg)
The most significant danger is the formation of permanent blindness, which occurs suddenly if the circulation in the optic nerve is interrupted. Usually, the patient has pain in the jaw, masticatory muscles, and tongue while eating or speaking. Other symptoms are the same as in polymyalgia rheumatica.
Diagnosis and treatment
The doctor makes a diagnosis based on symptoms and examination and confirms it with a biopsy of the temporal artery that runs through the shadows. Blood tests are helpful and usually reveal an elevated erythrocyte sedimentation rate and anemia. Temporal arteritis causes blindness in 20% of untreated patients, so treatment should be started as soon as it is suspected.
Questions and answers
Which diseases are characterized by vasculitis?
Vasculitis is characterized by:
- Henoch-Schonlein purpura,
- erythema nodosa,
- polyarteritis nodosa,
- temporal arteritis and
- Takayasu arteritis.
What are the symptoms of polymyalgia rheumatica?
Polymyalgia rheumatic causes severe pain and stiffness in the neck, shoulders, and hips. Stiffness is worse in the morning and after periods of rest. Muscular symptoms are accompanied by fever, uncharacteristic discomfort, weight loss, and depression. All these symptoms can appear either suddenly or gradually.
How common is vasculitis in Slovenia? p>
The estimated annual incidence rate was 5.1 per 100,000 adults, 6.1 per 100,000 men, and 3.7 per 100,000 women [1].
Is vasculitis a chronic disease?
Most forms of vasculitis are chronic, with periods of relapses and remissions[2].
Is vasculitis curable?
There is no cure for vasculitis, but early diagnosis and treatment are vital in relieving symptoms and slowing disease progression[3].
Sources and references
An extensive health manual for home use, Youth Book Publishing House
- Incidence of IgA vasculitis in the adult Slovenian population - https://pubmed.ncbi.nlm.nih.gov
- General Vasculitis - https://www.vasculitisfoundation.org
- Vasculitis - https://www.brighamandwomens.org