Urinary incontinence or otherwise loss of voluntary control over bladder function. The severity of this type of health problem ranges from the occasional dripping of urine when you cough or sneeze, for example, to a sudden and strong urge to urinate while not being able to get to the toilet in time.
INCONTINENCE: What is urinary incontinence? | Symptoms of incontinence | A visit to the doctor | Types of incontinence | Causes of incontinence | Diagnostics | INCONTINENCE TREATMENT | Conventional treatment | Alternative Methods | Treatment at home | Questions and Answers | Sources/references
Urinary incontinence is not a natural part of aging, even though incontinence occurs more frequently as a person ages. Most people can manage their urinary incontinence symptoms with a simple diet, lifestyle adjustments, or medical help. However, don't delay seeing a doctor if urinary incontinence prevents you from doing your daily tasks.
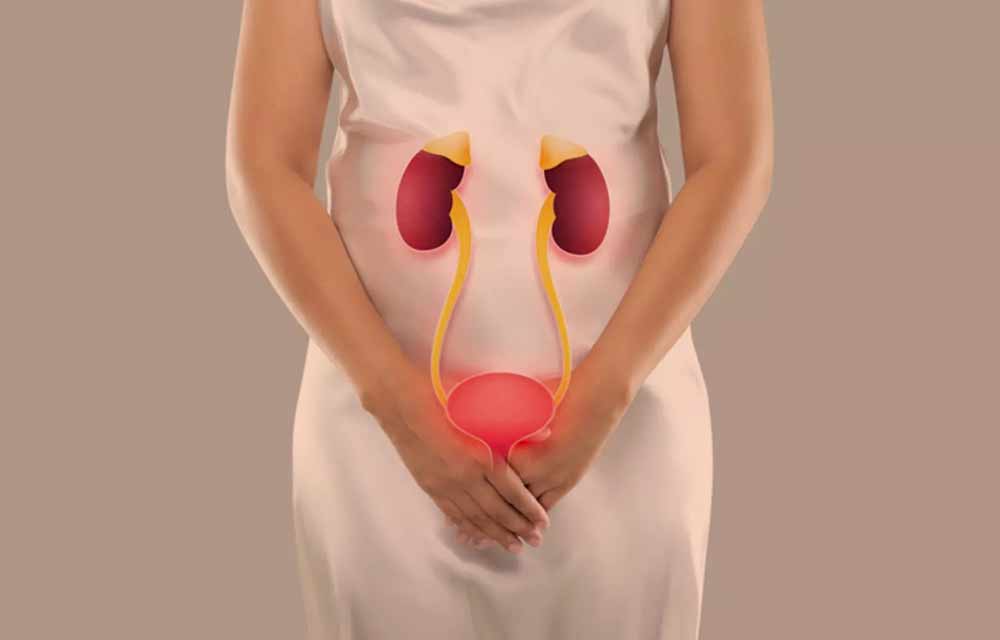
Image: Urinary incontinence is a severe and unpleasant health problem.
Most people experience occasional, minor leakage of urine, but some individuals may experience more frequent leakage of small to moderate amounts of urine.
The risk of developing incontinence may increase with age if you have a chronic medical condition, have given birth, have gone through menopause, have an enlarged prostate, or have had prostate cancer surgery.
Talking to your doctor over time about the risks of incontinence and how to manage it without compromising your quality of life is essential.
Incontinence - the involuntary passing of urine - is often associated with age, but contrary to popular belief, it is not an inevitable consequence of aging. It indicates another disease and can be treated, even in the elderly. With appropriate treatment, it can be cured or at least improved in around 70% of patients.

Without treatment, the condition does not improve; it can even worsen. Bladder and other urinary tract infections occur due to incontinence. In addition, the constant presence of urine on the skin causes unpleasant rashes and other skin diseases. Patients whose unsuccessful treatment can avoid such complications by using special absorbent pads and other devices designed to alleviate these problems.
The problem occurs more often in women than men, partly because with age or after childbirth, the pelvic floor muscles weaken and sag, allowing urine to leak.
Symptoms of urinary incontinence
- Inability to control urination.
- Involuntary urination during coughing, laughing, sneezing, running, or other physical activity.
Consult your doctor if:
- Lose control over urination after getting over illnesses such as bladder infections or after taking new medications. A sudden loss of control over urination can be a sign of nerve damage,
- Treatment methods that you try on your own do not help.
KEGGING EXERCISES

Women with stress incontinence can use Kegel exercises to strengthen the pelvic floor muscles, which support the uterus and bladder and regulate the contraction of the vagina and urethra. For example, slowly squeeze your pelvic floor muscles while urinating to stop urine flow. Hold for 10 seconds. Repeat several times. You can do the exercises even when you are not urinating - standing, sitting, or lying down.
Performing Kegel exercises can solve many problems related to urinary incontinence.
Types of urinary incontinence include:
- Stress incontinence: urine leaks when you put pressure on the bladder, such as when you cough, sneeze, laugh, exercise, or lift heavy objects.
- Urge incontinence: You have a sudden, strong urge to urinate, followed by involuntary urine leakage. You may feel the need to urinate frequently, even at night. Urge incontinence can be caused by a less problematic condition, such as an infection, or a more severe condition, such as a neurological disorder or diabetes.
Video content: urinary incontinence - what is it, different types of incontinence

- Overflow incontinence: means frequent or continuous urine dripping due to an incompletely emptied bladder.
- Functional incontinence: a physical or mental impairment that prevents you from getting to the toilet on time. If you have severe arthritis, you may be unable to unbutton your pants fast enough.
- Total incontinence: Your bladder cannot store urine, causing you to urinate constantly or experience frequent leakage.
- Mixed incontinence: You have more than one type of urinary incontinence – most often, this refers to a combination of stress and urge incontinence.
Causes of the development of urinary incontinence
The urinary system consists of the kidneys, the urethra, the urethra, and the bladder in the lower abdomen.
Muscles in the bladder contract to push urine into the urethra during urination. At that moment, the muscles that seal the urethra relax, allowing urine to leave the body.
Urinary incontinence can occur when these muscles don't work as they should.
Not all incontinence is long-lasting; some is a temporary phenomenon that ends when the cause disappears. Vaginal infections can also cause temporary incontinence.
Bladder irritation, medications, constipation, and limited mobility can cause incontinence. In addition, urinary tract infections (UTIs) are a common cause of temporary incontinence and should be taken seriously.
Incontinence can occur for a variety of reasons, and these reasons can be different for men and women. However, several causes of transient health problems generally go away when treated. In addition, when the disease is treated in certain situations, incontinence often disappears.
Video content: urinary incontinence - causes and symptoms

Long-term (chronic) health problems can cause incontinence. When you have leakage problems due to a chronic disease, you usually have to deal with them for a long time.
Chronic conditions don't usually improve with therapy, which means you may eventually have to learn to manage incontinence as a symptom of your chronic disease.
Temporary or short-term causes of incontinence can be:
- Urinary tract infections: An infection in the urinary tract (urethra, urethra, bladder, and kidneys) can cause pain and increase the need to urinate more often. After treatment, the urge to urinate usually disappears.
Image: urinary tract infection is still related to urinary incontinence

- Pregnancy: During pregnancy, your uterus puts extra pressure on your bladder as it expands. Most women who experience incontinence during pregnancy notice that the incontinence resolves within a few weeks after delivery.
- Medications: Incontinence can be a side effect of taking certain medications, including diuretics and antidepressants.
- Beverages: Some drinks, such as coffee and alcohol, can make you want to urinate more. Limiting your consumption of these drinks will usually decrease your need to urinate often.
- Constipation: chronic constipation (hard and dry stools) can cause bladder control problems.
Chronic or long-term causes for resulting incontinence can be:
- Pelvic floor disorders: If you have problems with your pelvic floor muscles, it can affect how your organs work, including your bladder.
- Stroke: A stroke can cause problems with muscle control. This may also include the muscles that regulate your urinary system.
- Diabetes: If you have diabetes, your body produces more urine. This increase in urine volume can cause leakage problems. In addition, peripheral neuropathy can affect bladder function.
- Menopause: Menopause is another cascade of changes in a woman's body when hormone levels change rapidly, and pelvic floor muscles can weaken.
- Multiple Sclerosis (MS): If you have MS, you may lose control of your bladder, causing problems with passing.
Video content: Multiple sclerosis - a personal story.

- Enlarged prostate: When the prostate is more significant than usual, it can cause more problems with bladder control. This condition is also called benign prostatic hyperplasia.
- The period after prostate cancer surgery: During prostate cancer surgery, the sphincter muscle can sometimes be damaged, causing stress incontinence.
The control of urination involves the entire urinary system - kidneys, ureter, bladder, urethra, pelvic floor muscles - and the central nervous system. For example, when the bladder is complete, it sends a message to a nerve in the spinal cord, which triggers what's known as the micturition reflex: the contraction of the bladder muscles that force urine into the urethra and out of the body. Incontinence occurs when any part of this complex process is disturbed.
Medical experts classify incontinence into three main groups, although many patients - especially women - experience symptoms from more than one group. In stress incontinence, the muscles surrounding the urethra are so weakened that they cannot resist a sudden increase in bladder pressure. Coughing, sneezing, laughing, exercising, or other types of movement that cause sudden pressure on the bladder cause urine to leak - usually just a few drops.
In urgent incontinence, the bladder begins to contract when it is complete, as in babies and young children; the patient has no control over the sudden urge to urinate. Although this type of incontinence is common in healthy people, it also occurs in patients with diseases of the central nervous system, such as stroke, Alzheimer's disease, Parkinson's disease, and multiple sclerosis. As a result, more urine escapes, emptying the bladder.
Overflow incontinence occurs when the patient no longer feels when he has to urinate. When the bladder is complete, excessive urine flows out, usually a small amount. The bladder is never completely emptied; at least some urine remains in it. This type of incontinence is associated with diabetes and in men with an enlarged prostate that obstructs urine flow; in women, the cause may be a fibroid or ovarian tumor. Drugs and neurological diseases of the bladder also cause it.
Video content: description of borderline incontinence

After surgical procedures on or near the urinary tract, scars or other injuries that cause incontinence are sometimes left behind. A slipped disc also causes urine to leak if it presses on the nerves that carry messages from or to the bladder.
In women, the muscles needed to control urination stretch and weaken during pregnancy and childbirth; the result may be incontinence. Research has shown that the more times a woman has given birth, the more likely she is to leak urine during exercise. After menopause, the concentration of the hormone estrogen in the blood decreases, which causes the tissues of the urinary tract to thin and the pelvic floor to weaken; incontinence may occur.
Incontinence is a possible side effect of diuretics, sedatives, antidepressants, antihistamines, and other drugs. Sometimes it can be cured just by changing the medicine. Talk to your doctor.
DIAGNOSTIC PROCEDURES
To determine the cause of your problems, the doctor will thoroughly question your previous and current illnesses, especially the symptoms - e.g., how often you urinate and how much urine you pass in one urination. He will then take a urine sample to rule out a possible infection. He will also examine the rectum, genitals, and abdomen to rule out tumors and an enlarged prostate. Finally, he'll tell you to cough to see if a few drops of urine escape as you do - a sign of stress incontinence. To prove borderline incontinence, a catheter may be inserted into your bladder after urination to see if any urine is left in it.
Video content: diagnosis of urinary incontinence and related problems

If standard treatments for incontinence don't help, or your doctor thinks surgery will help, he'll refer you to a specialist, usually a urologist, for further testing. A standard test is to measure urine flow: you will drink some liquid to fill your bladder, then you will urinate into a particular device that measures the flow. Cystometry is also helpful, a rather unpleasant procedure in which tubes are inserted into the bladder and rectum to measure the pressure that develops in the bladder muscles.
HEALING
Most incontinent patients can be cured or at least significantly improved with treatment. Both conventional and alternative medicine have effective treatments. Many conventional medicine doctors, e.g., two unconventional methods, are recommended for patients with stress incontinence - Kegel exercises and biofeedback. If you want, try alternative treatments first. If the incontinence does not improve or worsens, see a doctor to assess the condition and make the correct diagnosis.
CONVENTIONAL MEDICINE
Before prescribing drugs, many doctors advise on techniques to change behavioral patterns. Such treatment is safer than drugs and usually just as effective. Muscle strengthening, Kegel exercises, and biofeedback are most often prescribed.
Bladder training is also a helpful method. For seven days, record how much you drink, how often you urinate, and how much you urinate. Then start urinating at scheduled intervals, usually 30 to 60 minutes apart. Gradually, over several weeks, you can increase the time between visits to the toilet.
Video content: treatment of urinary incontinence

If your doctor determines that medication is necessary for your condition, he will select it based on the cause of the incontinence. You will be given antibiotics, for example, if there are signs of infection during the urine test. Postmenopausal women can receive hormone replacement therapy, which increases the concentration of estrogen in the blood (although the benefits of such treatment are not confirmed). For stress incontinence, they prescribe pseudoephedrine, ephedrine, or phenylpropanolamine, drugs that strengthen the sphincter, the circular muscle around the urethra that regulates urination. Propantheline bromide, imipramine, or oxybutynin chloride are effective for reducing the involuntary contraction of the bladder, which is characteristic of urge incontinence; these drugs allow the muscles involved in urination to function normally.
Some patients with stress incontinence are helped by a pessary inserted into the vagina and supports the pelvic floor muscles. The decision to use a pessary must be made by a doctor and prescribed for you.
A newer treatment for stress incontinence in women is to strengthen weakened pelvic muscles with small, conical weights that you insert into the vagina and train with them like you train other muscles with handles. Insert the lightest weight into the vagina with the tip down and squeeze the muscles for several minutes to prevent the weight from falling out. When you can hold the weight in your vagina for 20 to 30 minutes, try a heavier weight - and so on for several weeks. This gradually strengthens the muscles of the pelvic floor to their previous capacity.
If none of the described treatment methods help, your doctor may suggest surgery. An operation in which they repair damaged muscles and ligaments or place the bladder on their own is a place, is very effective in women with incontinence, especially stress incontinence, caused by pregnancy and childbirth. They can also implant an artificial sphincter; you open and close the device manually, thereby regulating the flow of urine and preventing leakage.
When there is no way to cure incontinence, you learn to live with the problem. For this, they have developed special tools, e.g., underwear that absorbs liquid and odor or devices that intercept urine and channel it into sealed plastic bags. Discuss these options with your doctor.
Treatment or relief of incontinence
- Medications: Over-the-counter and prescription medications can relax the muscles and nerves of the urinary tract and prevent bladder contractions. Botox can also help calm the bladder when, for example, other medications don't work. In addition, Botox can calm the symptoms and keep them under control for up to 6 months.
- Surgery: Your doctor may suggest surgery if your symptoms are severe and other treatments are not helping.
- Devices: a pessary is a ring that is inserted into a woman's vagina to position the urethra in a different position and thereby prevent urine leakage.
- Bladder training: By using the toilet at certain times, instead of waiting for the urge to urinate, you can slowly gain control of your bladder and increase the time between toilet visits.
- Kegel exercises: squeezing the pelvic floor muscles can help strengthen the bladder muscles and prevent urine leakage.
- Biofeedback: an electrical patch is placed on the skin over the bladder and urethra. This is connected to a monitor so you can watch when the muscles are contracting. This will help you learn to control them and prevent leakage.
Video content: Biofeedback techniques for performing exercises and strengthening the pelvic floor muscles.

- Nerve stimulation sends quick pulses of electrical energy to the muscles around the bladder, which can help strengthen them.
- Drink plenty of water: Drinking water infrequently can worsen the incontinence problem. Aim for at least six to eight glasses of water a day.
- Watch your diet: Reducing the amount of alcohol, carbonated drinks, coffee, and spicy and acidic foods can improve your symptoms.
- Lose weight: Losing extra pounds can improve incontinence; even a 5% weight loss can help.
- Quit smoking: Quitting smoking will increase your chances of reducing urine leakage.
ALTERNATIVE MODES
Most alternative treatments for incontinence focus on strengthening the pelvic floor muscles to support the bladder and thus control urination better.
ACUPUNCTURE
Acupuncturists believe that incontinence is the result of kidney and spleen qi deficiency. So they stimulate the points associated with these organs and their channels to restore the balance of chi in the affected areas. See an acupuncture specialist.
BIOFEEDBACK
Research has shown that 25% of patients with incontinence can regain complete control of their bladder with biofeedback techniques, and the condition improves significantly in 30-50% of patients. The treatment occurs by inserting a catheter into the bladder through the urethra, then slowly filling the bladder with liquid. At the same time, the patient learns to control the need to urinate using the biofeedback technique.
CHINESE HERBS
Golden lock tea, made from many herbs, is sometimes recommended to treat incontinence. Traditional Chinese herbalists believe that it helps the body retain fluids.
CHIROPRACTIC
By aligning the bones and joints of the pelvis, the urinary tract muscles are strengthened, improving bladder control.
Video content: Chiropractic and bladder problem relief.

Osteopaths also offer similar treatment.
HOMEOPATHY
Homeopaths have many remedies to treat incontinence. Their choice depends on the cause of incontinence. Some that are more often prescribed are:
- For stress incontinence, especially in the elderly, caustic, which is supposed to restore vitality to aging tissues;
- In stress and urge incontinence, pulsatilla calms the irritated mucous membrane of the urinary tract. It allows it to function well, especially when urine leaks when the patient gets up from lying on his stomach.
Consult a homeopathy specialist about other medicines.
NUTRITION
Try to maintain an average body weight. Excessive body weight puts pressure on the bladder muscles and weakens them.
Bladder muscles can also be weakened by the straining that accompanies constipation. Prevent constipation by increasing the fiber in your diet: eat more whole grains, fruits, and vegetables.
Avoid alcohol, caffeine, sugar, spicy food, and sour fruits and juices - they irritate the bladder and trigger urine leakage.
REFLEXOLOGY
Reflexologists treat those areas of the foot that stimulate the ureters, bladder, kidneys, adrenal glands, and the lower part of the spinal cord.
HEALTH AT HOME
- Prevent constipation: eat plenty of grains, fruits, and vegetables.
- Does Kegel exercises every day?
- Train yourself to urinate at longer intervals. Aim for three to six-hour intervals between toilet visits.
- Don't smoke. Nicotine irritates the bladder.
Video content: Stress, incontinence, and self-help at home.

- Wet twice: wait a few seconds after urinating, then try again.
- If you are a woman with stress incontinence, try crossing your legs when you sneeze or cough. Recent research has shown that this simple procedure effectively prevents urine leakage.
- If all treatment methods fail, buy special tools. For example, underwear, inserts, and protective pads absorb liquid and odor well. Try different brands until you find the one that suits you best.
Questions and Answers
What is the leading cause of urinary incontinence?
Incontinence can occur for many reasons related to urinary tract infection, vaginal infection, irritation, or constipation. In addition, some medications can cause bladder control problems that only last for a short time. If incontinence lasts longer, it may be due to: weak bladder sphincter muscles or pelvic floor[1].
How to eliminate urinary incontinence?
For many people with urinary incontinence, the following self-help tips and lifestyle changes are enough to relieve symptoms.
- Do pelvic floor exercises daily...
- stop smoking. ...
- do the appropriate exercises...
- avoid lifting loads...
- lose excess body weight...
- fix any closure...
- reduce caffeine intake...
- reduce alcohol intake[2].
What are the three treatment options for incontinence?
Incontinence products:
- Absorbent products such as panties or pads.
- Hand urinals.
- a catheter (a thin tube inserted into your bladder to drain urine)
- devices that are inserted into the vagina or urethra to prevent leakage of urine - for example, during exercise[3].
Sources and references
Source: Family Health Guide. Conventional and alternative treatment, Dr. Jaro Lajovic, Publishing House Mladinska knjiga
1. Urinary Incontinence in Older Adults - https://www.nia.nih.gov
2. 10 ways to stop leaks - https://www.nhs.uk
3. Non-surgical treatment - Urinary incontinence - https://www.nhs.uk










 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

