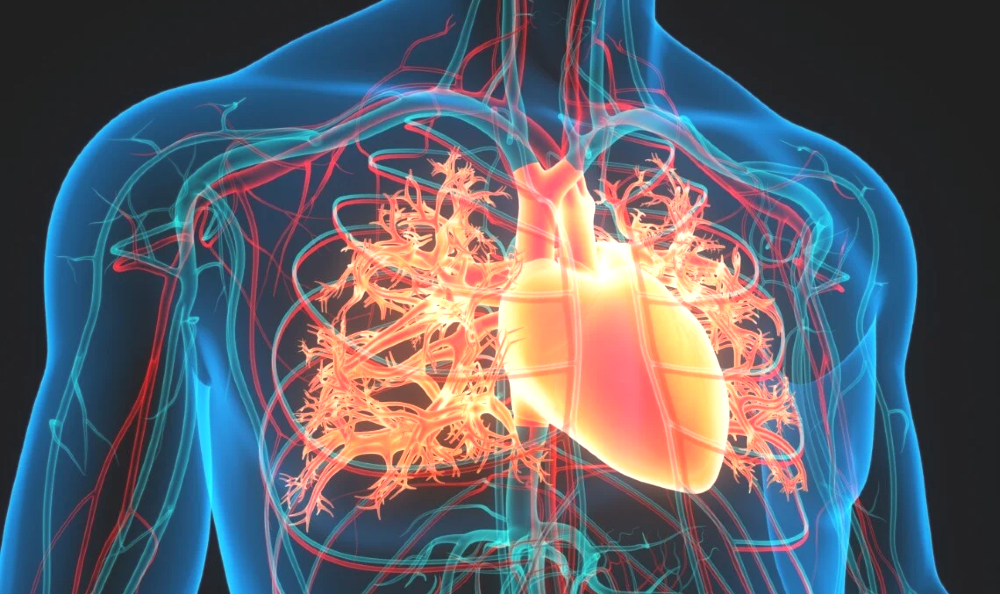
Aorta, največja arterija v telesu, sprejema kri, ki jo iztisne levi prekat, in jo vodi po vsem telesu, razen v pljuča. Kot veliko drevo se na poti od levega prekata do spodnjega dela trebuha v predelu medenice razvejuje v manjše veje.
ANEVRIZMA: Splošno | Anevrizme | Anevrizme trebušne aorte | Simptomi | Diagnoza | Zdravljenje | Anevrizme prsne aorte | Simptomi | Diagnoza | Zdravljenje | Disekcija aorte | Razumevanje aortne disekcije | Simptomi | Diagnoza | Zdravljenje | Prognoza | Bolezni ven in limfnih žil | Vprašanja in odgovori | Viri/reference
Med spremembami, ki prizadenejo aorto, so šibka mesta v njeni steni, ki omogočajo nastanek razširitev (anevrizem), zunanje raztrganine in krvavitev ter ločitev plasti aortne stene (disekcija).
Slika: Prikaz aorte in njenih velikih vej.
Anevrizme
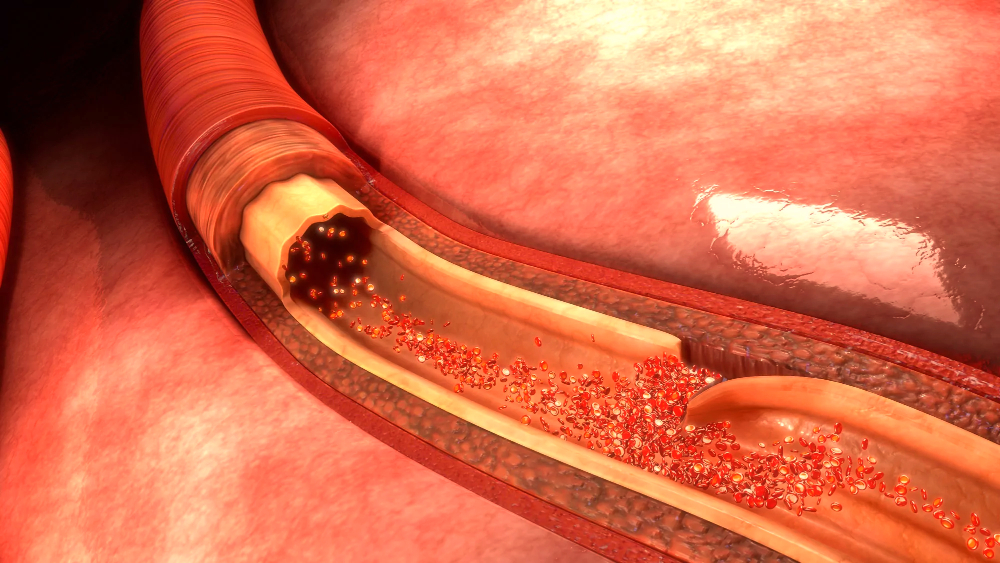
Anevrizma je razširitev arterijske stene, po navadi stene aorte. Razširitev se po navadi pojavi na šibkem predelu stene. Čeprav se lahko anevrizme razvijejo kjerkoli vzdolž aorte, se jih tri četrtine pojavi v trebušnem odseku. Anevrizme so lahko vrečaste (sakularne) ali vretenaste (fuziformne). Večina je vretenastih. Aortne anevrizme nastanejo predvsem zaradi arterioskleroze, ki v tolikšni meri oslabi aortno steno, da jo tlak v žili izboči navzven.
V anevrizmi pogosto nastane krvni strdek (tromb), ki se lahko širi ob njeni celotni steni. Visok krvni tlak in kajenje povečujeta nevarnost anevrizem. Nagnjenost k anevrizmam stopnjujejo poškodbe, vnetne bolezni aorte, dedne vezivnotkivne bolezni, npr. Marfanov sindrom in sifilis. Pri bolnikih z Marfanovim sindromom je anevrizma najpogostejša v navzgornjem delu (delu, ki izhaja iz srca in poteka navzgor).
Slika: Aortne anevrizme nastanejo predvsem zaradi arterioskleroze.
.jpg)
Anevrizme se lahko razvijejo tudi na drugih arterijah, ne samo na aorti. Številne nastanejo zaradi prirojene šibkosti ali arterioskleroze; druge so posledica vbodnih ali strelnih poškodb ali pa bakterijskih ali glivičnih okužb v arterijski steni. Okužba se po navadi začne drugod v telesu, največkrat na srčni zaklopki. Okužene anevrizme na arterijah, ki vodijo v možgane, so posebno nevarne, zato je pomembno zgodnje zdravljenje. Zdravljenje pogosto obsega kirurško popravo, ki pa je zelo tvegana.
Anevrizme trebušne aorte
Anevrizme v območju aorte, ki poteka skozi trebuh, se pogosto pojavljajo v družini. Mnogokrat se razvijejo pri ljudeh z visokim krvnim tlakom. Takšne anevrizme pogosto preše, žejo širino 8 cm in se lahko raztrgajo (normalen premer aorte je od 2 do 2,5 cm).
Simptomi
Osebe z anevrizmo trebušne aorte pogosto zaznajo utripajoč občutek v trebuhu. Anevrizma lahko povzroča bolečino, ki je praviloma globoka, predirna in se pojavlja predvsem v hrbtu! Lahko je huda in je po navadi stalna, čeprav sprememba položaja telesa nekaterim bolnikom ublaži bolečino. Prvi znak pretrganja je po navadi silovita bolečina v spodnjem delu trebuha in hrbta ter občutljivost v predelu nad anevrizmo. Pri hudi notranji krvavitvi bolnik hitro zapade v šok. Pretrganje trebušne anevrizme je pogosto usodno.
Diagnoza
Bolečina je poveden, toda pozen znak. Veliko ljudi z anevrizmo pa nima simptomov in jim spremembo po naključju odkrijejo med običajnim zdravniškim pregledom ali pri rentgenskem slikanju, potrebnem zaradi česa drugega. Zdravnik po navadi otiplje utripajočo gmoto sredi trebuha. Anevrizme, ki se hitro večajo in bi se lahko kmalu pretrgale, so med pregledom trebuha pogosto boleče ali občutljive za pritisk. Pri debelih ljudeh včasih ni mogoče odkriti niti velikih anevrizem.
Video vsebina: Razumevanje anevrizme trebušne aorte.

Pri diagnosticiranju anevrizem lahko koristi več preiskav. Rentgensko slikanje trebuha razkrije anevrizmo, ki ima v steni odložke kalcija. Ultrazvočni pregled po navadi jasno prikaže velikost anevrizme. Še natančneje pokaže velikost in obliko anevrizme računalniški to-mogram trebuha, zlasti če je narejen po intra-venskem vbrizganju kontrastnega sredstva, vendar je ta preiskava dražja. Natančno je tudi magnetnoresonančno slikanje, ki pa je dražje od ultrazvočnega pregleda in je le redko potrebno.
Zdravljenje
Če anevrizma ni na tem, da se pretrga, je zdravljenje odvisno od njene velikosti. Anevrizme, ki imajo v premeru manj kot 5 cm, se le redko pretrgajo, če pa velikost preseže 6 cm, je nevarnost mnogo večja. Zato zdravniki po navadi priporočajo operacijo anevrizem, ki merijo nad 5 cm, razen če je poseg zaradi siceršnjega zdravstvenega stanja preveč tvegan. Med operacijo na žilo namestijo sintetični presadek, da popravijo anevrizmo. Umrljivost pri takšnih posegih je približno 2-odstotna.
Slika: Pretrganje trebušne anevrizme je pogosto usodno.
.jpg)
Pretrganje ali grozeče pretrganje trebušne anevrizme zahteva nujno operacijo. Tveganje, da bo bolnik med operacijo zaradi raztrgane anevrizme umrl, je približno 50-odstotno. Če se anevrizma raztrga, so zaradi motene prekrvitve ali šoka, povezanega z izgubo krvi, ogrožene ledvice. Če se po operaciji razvije ledvična odpoved, so možnosti za preživetje zelo slabe. Nezdravljeno pretrganje anevrizme je vselej usodno.
Anevrizme prsne aorte
Četrtina vseh aortnih anevrizem nastane v območju aorte, ki poteka skozi prsni koš. Posebno pogosta oblika anevrizem prsne aorte je razširitev na mestu, kjer aorta zapušča srce. Povečanje lahko povzroči nepravilno delovanje zaklopke med srcem in aorto (aortne zaklopke), zato začne zaklopka puščati (ko se zapre, del krvi steče nazaj v prekat). Približno 50 odstotkov bolnikov s to spremembo ima Marfanov sindrom ali njegovo različico. Pri preostalih 50 odstotkih sprememba nima jasnega vzroka, toda številni od teh bolnikov imajo visok krvni tlak.
Simptomi
Anevrizme prsne aorte lahko postanejo velikanske, pri tem pa ne povzročajo simptomov. Simptomi se pojavijo zaradi pritiska razširjene aorte na okolico. Značilni so bolečina (po navadi v zgornjem delu hrbta), kašelj in piskajoče dihanje. Bolnik lahko izkašljuje kri zaradi pritiska na sapnik ali bližnje dihalne poti ali razjede na njih. Pritisk na požiralnik, po katerem hrana prehaja v želodec, včasih oteži požiranje.
Pritisk na živec, ki oživčuje grlo, povzroči hripavost. Bolnik lahko doživi skupek simptomov (Homerjev sindrom), ki obsega zoženo zenico, povešeno veko in znojenje samo na eni strani obraza. Rentgenogram prsnih organov lahko pokaže odrinjen sapnik. Tudi nenormalno utripanje stene prsnega koša je lahko znak anevrizme prsne aorte.
Video vsebina: Vprašanja in odgovori o anevrizmah torakalne aorte.

Če se anevrizma prsne aorte pretrga, se visoko v hrbtu po navadi pojavi silovita bolečina. Ko raztrganje napreduje, se lahko bolečina širi navzdol po hrbtu in v trebuh. Bolnik jo lahko čuti tudi v prsih in rokah, kar posnema bolečino pri srčnem infarktu. Prizadeti lahko hitro zapade v šokA in umre zaradi izkrvavitve.
Diagnoza
Zdravnik diagnosticira anevrizmo prsne aorte po simptomih ali jo po naključju odkrije med pregledom. Anevrizmo lahko razkrije rentgenogram prsnih organov, narejen zaradi kakšnega drugega vzroka. Za ugotovitev natančne velikosti anevrizme se uporablja računalniška tomografija (CT), magnetnoresonančno slikanje (MRS) ali ultrazvočni pregled skozi požiralnik (transezofagealni ultrazvok). Aortografija, rentgensko slikanje po vbrizganju kontrastnega sredstva (ki prikaže obrise anevrizme), zdravnikom po navadi pomaga pri odločitvi, ali je potrebna operacija in kakšna.
Zdravljenje
Če je anevrizma prsne aorte širša od 7 cm, se zdravniki po navadi odločijo za kirurško popravo s sintetičnim vsadkom. Ker je pri bolnikih z Marfanovim sindromom nevarnost, da se bo raztrgala, večja, pride operacija v poštev že pri manjših anevrizmah. Tveganje, da bo bolnik med popravljanjem anevrizme prsne aorte umrl, je veliko - od 10- do 15-odstotno. Zato zdravnik lahko predpiše zdravljenje z zaviralcem beta, da bi srčni utrip upočasnil in krvni tlak znižal do te mere, da bi zmanjšal nevarnost raztrganja.
Disekcija aorte
Disekcija aorte (disekantna anevrizma) je pogosto usoden dogodek, pri katerem se notranja plast aortne stene pretrga, zunanja pa ostane cela; kri steče skozi raztrganino, razkolje (dise-cira) srednjo plast in ustvari nov kanal v steni aorte.
Razumevanje aortne disekcije
Pri disekciji aorte se notranja plast aortne stene pretrga, kri steče skozi raztrganino, pri tem razcepi srednjo plast in v steni ustvari nov kanal (disekcija). Prizadetost arterijske stene je odgovorna za večino disekcij aorte. Najpogostejši vzrok takšne prizadetosti je visok krvni tlak; imata ga dve tretjini ljudi, pri katerih se razvije disekcija aorte.
Slika: Prizadetost arterijske stene je odgovorna za večino disekcij aorte.
Med drugimi vzroki so dedne bolezni vezivnega tkiva, zlasti Marfanov in Ehlers-Danlosov sindrom, prirojene hibe srca in žil (npr. koarktacija aorte, odprti arteriozni duktus in napake aortne zaklopke), arterioskleroza in poškodbe. V redkih primerih se disekcija razvije po naključju, ko zdravnik v arterijo vstavlja kateter (npr. pri aortografiji ali an-giografiji) ali operira srce oz. žile.
Simptomi
Skoraj vsakdo, ki doživi disekcijo aorte, občuti bolečino - praviloma se pojavi nenadoma in je silovita. Najpogosteje bolniki občutijo trgajočo ali parajočo bolečino v prsih. Pogosta je tudi v hrbtu med lopaticama. Bolečina po-gosto spremlja napredovanje disekcije, ko se ta širi vzdolž aorte. Ko disekcija napreduje, lahko zapre iztoči-šče ene ali več arterij, ki izvirajo iz aorte. Glede na to, katere arterije se zamašijo, se kot posledica lahko pojavijo možganska kap, srčni infarkt, nenadna bolečina v trebuhu, okvara živcev, ki povzroči mravljinčenje, in nezmožnost za premikanje uda.
Diagnoza
Diagnoza disekcije aorte je zdravnikom zaradi značilnih simptomov po navadi očitna. Med telesnim pregledom pri približno dveh tretjinah ljudi z disekcijo aorte ugotovijo oslabljen ali odsoten pulz na rokah oz. nogah. Disekcija, ki se širi nazaj proti srcu, lahko povzroči šum, ki je slišen s stetoskopom. Kri se lahko nabira v prsnem košu. Kri, ki skozi disekcijo izteka okrog srca, včasih prepreči normalno bitje srca in povzroči tamponado; ta je smrtno nevarna.
Rentgenogram prsnih organov pri več kot 90 odstotkih simptomatičnih bolnikov pokaže razširjeno aorto. Ultrazvočni pregled po navadi potrdi diagnozo, tudi če aorta ni povečana. Računalniška tomografija (CT), opravljena po vbrizganju kontrastnega sredstva, je zanesljiva in jo je mogoče opraviti hitro, to pa je pomembno v nujnih primerih.
Zdravljenje
Bolnike z disekcijo aorte sprejmejo na intenzivni oddelek. Tam skrbno spremljajo njihove vitalne znake (pulz, krvni tlak, hitrost dihanja). Smrt lahko nastopi nekaj ur po začetku disekcije, zato zdravniki takoj, ko je mogoče, dajo zdravila, ki zmanjšajo srčni utrip in krvni tlak na najmanjšo možno mero, s katero je še zagotovljena zadostna prekrvitev možganov, srca in ledvic. Kmalu po začetku zdravljenja se mora zdravnik odločiti, ali je potrebna operacija ali kaže nadaljevati le zdravljenje z zdravili.
Video vsebina: Operacija disekcije aorte.

Zdravniki skoraj vedno priporočajo operacijo pri disekcijah v območju prvih desetih centimetrov aorte, najbližje srcu, razen če ni nevarnost operacije zaradi zapletov disekcije prevelika. Pri disekcijah, ki so od srca bolj oddaljene, po navadi nadaljujejo zdravljenje z zdravili, z izjemo disekcij, ki povzročajo iztekanje krvi, in disekcij pri osebah z Marfano-vim sindromom. V teh primerih je potrebna operacija.
Med operacijo kirurg odstrani čim večji del disecirane aorte, prepreči dotekanje krvi v napačno svetlino (kanal, nastal z ločitvijo plasti) in obnovi aorto s sintetičnim vsadkom. Če aortna zaklopka pušča, jo popravi ali zamenja.
Prognoza
Okrog 75 odstotkov nezdravljenih bolnikov z disekcijo aorte umre v prvih 2 tednih. V nasprotju s tem je 60 odstotkov zdravljenih bolnikov, ki preživijo prva 2 tedna, še vedno živih 5 let po zdravljenju, 40 odstotkov pa jih preživi vsaj 10 let. Od bolnikov, ki umrejo po prvih 2 tednih, jih približno tretjina podleže zapletom disekcije, preostali dve tretjini pa umreta zaradi drugih bolezni.
Umrljivost pri operacijah v velikih zdravstvenih centrih je zdaj okrog 15-odstotna pri aortnih disekcijah, ki so bližje srcu, in nekoliko večja pri tistih, ki so bolj oddaljene. Zdravniki vsem bolnikom z disekcijo aorte, tudi operiranim, dolgoročno dajejo zdravila za znižanje krvnega tlaka, da je aorta manj obremenjena. Zdravniki bolnike skrbno spremljajo zaradi možnih poznih zapletov; trije najpogostejši so ponovna disekcija, nastanek anevrizme na oslabeli aorti in napredujoče puščanje (insufi-cienca) aortne zaklopke. Pri vsakem od teh utegne biti potrebno kirurško zdravljenje.
Bolezni ven in limfnih žil
Po venah se kri iz vseh telesnih organov vrača v srce. Med poglavitnimi težavami, ki lahko prizadenejo vene, so vnetje, strdki in okvare, ki vodijo k razširjenju in krčnim žilam. Limfni sistem oblikujejo mezgovnice (limfne žile) s tanko steno, po katerih tekočina, beljakovine, minerali, hranila in druge snovi iz vseh organov odtekajo v vene.
Limfna tekočina (mezga) pri tem prehaja skozi bezgavke, ki zagotavljajo zaščito pred širjenjem okužb in raka, in se končno v območju vratu izlije v venski sistem. Poglavitne težave, povezane z limfnim sistemom, se pojavijo, če mezgovnice ne zmorejo odvesti vse tekočine, ki priteka vanje, če se zamašijo zaradi tiimnria ali če se vnameio.
Slika: Globoke vene igrajo pri potiskanju krvi navzgor pomembno vlogo.
.jpg)
Da kri teče navzgor, ne navzdol, so v globokih venah enosmerne zaklopke. Vsaka zaklopka ima dve polovici, lističa, ki se z robovi stikata. Potisnjena kri lističa razpre kot krili nihajnih vrat, kri, ki jo težnost potisne v nasprotno smer. Globoke vene igrajo pri potiskanju krvi navzgor pomembno vlogo. Ker ležijo med močnimi mečnimi mišicami, jih te pri vsakem koraku močno stisnejo. Tako kot npr. s stiskanjem tube iztisnemo zobno pasto, stiskanje globokih ven potiska kri navzgor. Po teh venah se v srce vrne 90 ali še več odstotkov krvi iz nog.
Vprašanja in odgovori
Katera vrsta anevrizme je najpogostejša?
Anevrizme aorte so daleč najpogostejše. Nastanejo v vaši aorti, največji arteriji vašega telesa. Vaša aorta prenaša kri iz srca. Anevrizme, ki se razvijejo v arterijah, ki niso vaša aorta, se imenujejo periferne anevrizme[1].
Ali je anevrizma v območju trebušne aorte težko ozdravljiva?
Manjše, počasi rastoče anevrizme aorte je mogoče zdraviti s čakanjem, spremembami življenjskega sloga in zdravili. Velike ali hitro rastoče anevrizme aorte lahko zahtevajo operacijo[2].
Kako lahko je zaznati disekcijo aorte?
Diagnoza disekcije aorte je zdravnikom zaradi značilnih simptomov po navadi očitna. Med telesnim pregledom pri približno dveh tretjinah ljudi z disekcijo aorte ugotovijo oslabljen ali odsoten pulz na rokah oz. nogah.
Kako se kažejo simptomi anevrizme prsne aorte?
Značilni simptomi so bolečina (po navadi v zgornjem delu hrbta), kašelj in piskajoče dihanje. Bolnik lahko izkašljuje kri zaradi pritiska na sapnik ali bližnje dihalne poti ali razjede na njih. Pritisk na požiralnik, po katerem hrana prehaja v želodec, včasih oteži požiranje. Pritisk na živec, ki oživčuje grlo, povzroči hripavost. Bolnik lahko doživi skupek simptomov (Homerjev sindrom), ki obsega zoženo zenico, povešeno veko in znojenje samo na eni strani obraza. Tudi nenormalno utripanje stene prsnega koša je lahko znak anevrizme prsne aorte.
Kakšne so lahko anevrizme?
Anevrizme so lahko vrečaste (sakularne) ali vretenaste (fuziformne). Večina je vretenastih.
Kako uspešna je operacija anevrizme?
Možnost preživetja je veliko večja, če imate operacijo pred rupturo. V tem primeru je možnost preživetja po operaciji anevrizme 95- do 98-odstotna. Odprta operacija je bolj tvegana za ljudi z drugimi resnimi zdravstvenimi težavami[3].
Kako dolgo traja okrevanje po operaciji anevrizme prsne aorte?
Nekaj tednov po operaciji se boste počutili bolj utrujeni kot običajno. Po 4 do 6 tednih boste morda lahko opravljali številne svoje običajne dejavnosti[4].
Viri in reference
Veliki zravstveni priročnik za domačo uporabo, Založba mladinska knjiga
- Aneurysm - https://my.clevelandclinic.org
- Abdominal Aortic Aneurysm - https://www.hopkinsmedicine.org
- Aneurysm Surgery: Traditional Open Surgery - https://my.clevelandclinic.org
- Thoracic Aortic Aneurysm Repair Surgery: What to Expect at Home - https://myhealth.alberta.ca





 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

