Bolezen koronarnih arterij (ali ishemična bolezen srca) je bolezen, pri kateri se v celicah notranje plasti koronarnih arterij nakopičijo maščobni odložki, ki ovirajo pretok krvi.
ANGINA PEKTORIS: Splošno | Angina pektoris | Vzroki | Simptomi | Maščobni odložki v koronami arteriji | Diagnoza | Holesterol in bolezen koronarnih arterij | Zdravljenje stabilne angine pektoris | Zdravljenje nestabilne angine pektoris | Vprašanja in odgovori | Viri/reference
Maščobni odložki (ateromi ali lehe) nastanejo postopoma in so razširjeni v velikih vejah dveh glavnih koronarnih arterij, ki kot venec obdajata srce in ga oskrbujeta s krvjo; po-stopno dogajanje, ki do tega privede, imenujemo ateroskleroza. Ateromi se bočijo v arterijsko svetlino in jo ožijo.
Ko se večajo, se njihovi deli lahko pretrgajo in pridejo v krvni obtok ali pa na njihovi površini nastanejo majhni krvni strdki.
Slika: Glavna zapleta bolezni koronarnih arterij sta angina pektoris in srčni infarkt.
.jpg)
Za normalno krčenje in črpanje krvi potrebuje srčna mišica (miokard) stalen dotok s kisikom bogate krvi iz koronarnih arterij. Ko zožitev koronarne arterije napreduje, se pojavi nezadostna prekrvljenost (ishemija), ki povzroči okvaro srca. Najpogostejši vzrok mi-okardne ishemije je bolezen koronarnih arterij; le-to imenujemo tudi ishemična bolezen srca. Glavna zapleta te bolezni sta angina pektoris in srčni infarkt.
Bolezen koronarnih arterij se pojavlja pri ljudeh vseh ras, posebno pogosta pa je med belci. Vendar rasa ni tako pomemben dejavnik tveganja kot je posameznikov življenjski slog. Nevarnost bolezni koronarnih arterij povečujejo zlasti izrazito mastna prehrana, kajenje in sedeč način življenja.
Tudi v Sloveniji so bolezni srca in ožilja vodilni vzrok smrti, bolezen koronarnih arterij pa je najpomembnejši posamezni vzrok teh bolezni. Umrljivost zaradi nje je pri moških večja kot pri ženskah, zlasti v obdobju med 35. in 55. letom; po tej starosti se tudi pri ženskah poveča.
Angina pektoris
Angina pektoris je prehodna bolečina ali tiščanje v prsih, ki se pojavi, če srčna mišica ne dobiva dovolj kisika. Potrebo srca po kisiku določa napornost njegovega dela: hitrost bitja in moč utripanja. Telesne in čustvene obremenitve povečajo delo srca in s tem tudi potrebo srca po kisiku. Če so arterije zožene ali zamašene in se pretok krvi v mišico ne more tako povečati, da bi zadovoljil povečano potrebo po kisiku, se pojavi ishemija in povzroči bolečino.
Vzroki
Po navadi je vzrok angine pektoris bolezen koronarnih arterij, čeprav ima lahko še druge vzroke, med drugim nepravilnosti aortne za-klopke, zlasti aortno stenozo (zožitev aortne zaklopke), aortno insuficienco (puščanje aortne zaklopke) in hipertrofično subaortno stenozo.
Ker je aortna zaklopka blizu ustja koronarnih arterij, te spremembe zmanjšajo pretok krvi skozi koronarne arterije. Prav tako lahko povzročijo angino pektoris arterijski spazmi (nenadni, prehodni arterijski krči), huda anemija pa zmanjša preskrbo srca s kisikom in tako izzove angino pektoris.
Simptomi
Angine pektoris ne doživljajo vsi, ki imajo ishemijo. Ishemijo brez angine pektoris imenujemo tiha ishemija. Ni znano, zakaj je ishemija včasih tiha. Najpogosteje občuti bolnik angino pektoris kot tiščanje ali bolečino za prsnico. Bolečina se lahko pojavi tudi v levi rami ali po notranji strani leve roke, v hrbtu, v vratu, spodnji čeljusti ali zobeh, včasih tudi po desni roki. Veliko bolnikov navaja nelagodje, ne bolečine.
Video vsebina: Angina pektoris - simptomi in patologija.

Praviloma angino pektoris izzove telesna dejavnost; po navadi ne traja več kot nekaj minut in med mirovanjem mine. Pri nekaterih ljudeh se pojavlja predvidljivo, pri določeni stopnji obremenitve. Pri drugih je nepredvidljiva.
Pogosto je hujša, če napor sledi obroku, in navadno je hujša v hladnem vremenu. Hoja v vetru ali prehod iz toplega prostora na mrzel zrak lahko sproži napad angine pektoris. Povzročijo ali poslabšajo jo lahko tudi čustveni pretresi. Včasih jo izzove močno čustvo tudi med mirovanjem ali moraste sanje med spanjem.
Variantna angina pektoris (imenovana tudi Prinzmetalova angina pektoris) nastane zaradi spazma ene od velikih koronarnih arterij na površini srca. Značilno zanjo je, da se bolečina pojavi med mirovanjem, ne med naporom, napad pa spremljajo določene elektro-kardiografske (EKG) spremembe. Nestabilna angina pektoris je tista, pri kateri se vzorec simptomov spreminja.
Ker značilnosti angine pektoris pri posameznem bolniku po navadi ostajajo stalne, je vsaka sprememba - npr. hujša bolečina, pogostejši napadi ali napadi med manjšim naporom ali celo med mirovanjem - resna. Takšno spreminjanje simptomov po navadi kaže na hitro napredovanje koronarne bolezni z naraščajočo zožitvijo arterije zaradi pretrganja ateroma ali nastanka krvnega strdka. Nevarnost srčnega infarkta je zelo velika in nestabilna angina je nujno stanje.
Maščobni odložki v koronami arteriji
Ko se v koronami arteriji nakopičijo maščobni odložki, se pretok krvi zmanjša in srčna mišica trpi pomanjkanje kisika. Pomanjkanje kisika v srčni mišici lahko povzroči resne težave in poškodbe srčnega tkiva.
Slika: Angina pektoris je lahko znak koronarne bolezni srca.
.jpg)
Zdravljenje pomanjkanja kisika v srčni mišici se osredotoča na odpravo osnovnega vzroka, kar pogosto zahteva zdravljenje koronarne bolezni srca, obnavljanje normalnega pretoka krvi in preprečevanje nadaljnjih poškodb srčne mišice.
Diagnoza
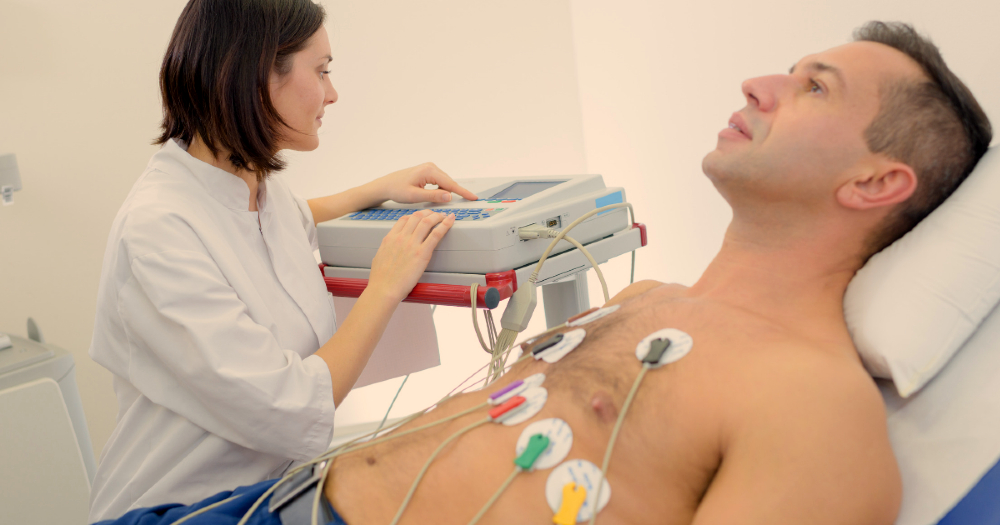
Zdravnik diagnosticira angino pektoris predvsem po bolnikovem opisu simptomov. V obdobju med napadi - in včasih celo med samim napadom angine - telesni pregled in EKG marsikdaj razkrijeta le malo nepravilnosti ali sploh nobene. Med napadom se lahko hitrost srčnega utripa nekoliko poveča, krvni tlak se lahko zviša in zdravnik lahko s stetoskopom sliši značilno spremenjeno bitje. Med napadom značilne angine pektoris so po navadi opazne spremembe v EKG, v obdobjih medposameznimi napadi pa je lahko EKG normalen, celo pri bolnikih z obsežnimi bolezenskimi spremembami na koronarnih arterijah.
Kadar so simptomi značilni, je diagnoza za zdravnika po navadi lahka. Vrsta bolečine, njena lega in njena povezanost z naporom, obroki, vremenom in drugimi dejavniki mu pomagajo postaviti diagnozo. Določene preiskave pomagajo ugotoviti izrazitost ishemije ter navzočnost in razširjenost bolezni koronarnih arterij. Obremenitveno testiranje (preiskava, pri kateri preiskovanec hodi po tekoči preprogi, medtem pa spremljajo njegov EKG) pomaga oceniti izrazitost koronarne bolezni in zmožnost srca, da se odzove na ishemijo.
Slika: EKG pomaga diagnosticirati tudi variantno angino pektoris.
Izsledki lahko pomagajo ugotoviti, ali je potrebna koronarna arteriografija ali operacija. Radioizotopsko slikanje v povezavi z obremenitvenim testiranjem marsikdaj zagotovi dragocene podatke o bolnikovi angini pektoris. Radioizotopsko slikanje ne le potrdi navzočnost ishemije, ampak tudi odkrije, kateri predel srčne mišice je prizadet in kako obsežen je, ter prikaže, kolikšen je dotok krvi v srčno mišico.
Obremenitvena ehokardiografija je preiskava, pri kateri naprava iz ultrazvočnih valov, odbitih od srca, ustvari slike (ehokardiograme). Preiskava je neškodljiva in prikaže velikost srca, gibanje srčne mišice, pretok krvi skozi srčne zaklopke in njihovo delovanje. Ehokardiograme naredijo med mirovanjem in pri največji obremenitvi. Če ima preiskovanec ishemijo, črpalno gibanje stene levega prekata ni normalno.
Koronarno arteriografijo včasih opravijo, če diagnoza bolezni koronarnih arterij ali ishemije ni zanesljiva. Pogosteje pa jo uporabijo, da ugotovijo izrazitosti koronarne bolezni in da ocenijo, ali bolnik potrebuje poseg za izboljšanje krvnega pretoka - obvodno operacijo koronarnih arterij ali angioplastiko. Pri maloštevilnih bolnikih z značilnimi simptomi angine pektoris in nenormalnim izvidom obremenitvenega testiranja koronarna arteriografija ne pokaže bolezenskih sprememb na koronarnih arterijah.
Pri nekaterih takšnih bolnikih so nenormalno zožene male arterije v srčni mišici. O tej bolezni, ki jo nekateri strokovnjaki imenujejo sindrom X, ostaja odprtih mnogo vprašanj. Po navadi se simptomi pri tem sindromu izboljšajo z jemanjem nitratov ali zaviralcev beta. Prognoza bolnikov s sindromom X je dobra. Dinamična elektrokardiografija s Holterjevim monitorjem (prenosnim snemalnikom EKG na baterije) pri nekaterih bolnikih odkrije nepravilnosti, ki nakazujejo tiho ishemijo.
Slika: Radioizotopsko slikanje potrdi navzočnost ishemije.
.jpg)
Mnenja o pomembnosti tihe ishemije niso povsem enotna, toda na splošno je izrazitost bolezni koronarnih arterij tista, ki določa stopnjo tihe ishemije in s tem prognozo. EKG pomaga diagnosticirati tudi variantno angino pektoris, ker odkrije določene spremembe, ki se pojavijo, če se napad razvije med mirovanjem. Angiografija (filmsko rentgensko slikanje arterij po vbrizganju kontrastnega sredstva) včasih odkrije spazem v koronarnih arterijah, na katerih ni ateromov. Nekaterim bolnikom med angiografijo vbrizgajo določena zdravila, da izzovejo spazem.
Holesterol in bolezen koronarnih arterij
Nevarnost bolezni koronarnih arterij se povečuje s povečevanjem koncentracije celotnega holesterola in holesterola majhne gostote (holesterola LDL; slabega holesterola) v krvi. Nevarnost pa se zmanjšuje z večanjem koncentracije holesterola velike gostote (holesterola HDL; dobrega holesterola).
Prehrana vpliva na koncentracijo celotnega holesterola - in tako tudi na nevarnost koronarne bolezni. Sodobna zahodnjaška prehrana povečuje koncentracijo celotnega holesterola. Sprememba prehrane (in jemanje predpisanih zdravil, če je potrebno) lahko zmanjša koncentracijo holesterola. Zmanjšanje koncentracije celotnega in slabega holesterola upočasni ali celo preobrne napredovanje koronarne bolezni.
Video vsebina: Če imate stabilno angino pektoris, bi morali opraviti postopek za odpiranje arterij?

Zmanjšanje koncentracije slabega holesterola najbolj koristi bolnikom, ki imajo še druge dejavnike tveganja za koronarno bolezen. Med takšne dejavnike spadajo kajenje, visok krvni tlak, debelost, telesna nedejavnost, velika koncentracija trigliceridov, genska predispozicija in moški steroidi (androgeni). Opustitev kajenja, znižanje krvnega tlaka, zmanjšanje teže in povečanje telesne dejavnosti zmanjšujejo tveganje za koronarno bolezen.
Prognoza
Med ključnimi dejavniki, ki omogočajo napoved, kaj se pri bolniku utegne zgoditi, so starost, obsežnost sprememb na koronarnih arterijah, izrazitost simptomov, predvsem pa stopnja normalnega delovanja srčne mišice. Kolikor bolj so koronarne arterije prizadete in kolikor bolj so zožene, toliko slabša je prognoza. Prognoza je presenetljivo dobra pri bolnikih s stabilno angino pektoris in normalno črpalno zmogljivostjo (prekatnim mišičnim delovanjem). Zmanjšana črpalna zmogljivost močno poslabša pričakovani potek.
Zdravljenje
Zdravljenje se začne s prizadevanjem za preprečitev bolezni koronarnih arterij, upočasnitev njenega napredovanja ali njeno nazadovanje z obvladovanjem znanih vzrokov (dejavnikov tveganja) zanjo. Primarne dejavnike tveganja, npr. zvišan krvni tlak in zvišano koncentracijo holesterola, je treba zdraviti takoj. Kajenje je najpomembnejši preprečljivi dejavnik tveganja za to bolezen.
Slika: Primarne dejavnike tveganja je potrebno zdraviti takoj.
.jpg)
Zdravljenje angine pektoris je deloma odvisno od izrazitosti in stabilnosti simptomov. Če so simptomi stabilni in blagi do zmerni, utegne biti najučinkovitejša pot odpravljanje dejavnikov tveganja in uporaba zdravil. Če se simptomi hitro slabšajo, se zdravniki po navadi odločijo za takojšen sprejem bolnika v bolnišnico in za zdravljenje z zdravili. Če simptomi kljub zdravilom, dieti in spremembam življenjskega sloga ne popustijo občutno, pride v poštev angiografija, ki omogoča presojo o možnosti za obvodno operacijo ali angiopla-stiko koronarne arterije.
Zdravljenje stabilne angine pektoris
Zdravljenje je zastavljeno tako, da prepreči ali zmanjša ishemijo in čim bolj zmanjša simptome. Na voljo so štiri vrste zdravil: zaviralci beta (blokatorji beta), nitrati, kalcijevi antagonisti in antiagregacijska zdravila.
Zaviralci beta zavirajo učinke hormonov adrenalina in noradrenalina na srce in druge organe. Med mirovanjem upočasnijo srčni utrip (frekvenco), med telesno obremenitvijo pa omejijo porast srčne frekvence in tako zmanjšajo potrebo po kisiku. Za zaviralce beta in nitrate je dokazano, da zmanjšujejo možnost srčnega infarkta in nenadne smrti in izboljšajo dolgoročni potek pri bolnikih s koronarno boleznijo.
Nitrati, npr. nitroglicerin, širijo žile. Uporabljati je mogoče kratkodelujoče ali dolgodelujo-če. Tableta nitroglicerina, položena pod jezik (sublingvalna uporaba), po navadi odpravi napad angine pektoris v 1 do 3 minutah; učinki tega kratkodelujočega nitratnega zdravila trajajo 30 minut. Bolniki s kronično stabilno angino pektoris bi morali vedno imeti pri sebi tablete ali pršilo nitroglicerina. Koristi lahko, če bolnik vzame tableto, tik preden doseže tisto raven obremenitve, za katero ve, da mu izzove napad angine.
Video vsebina: Simptomi in kako zdraviti napad angine.

Nitroglicerin je mogoče uporabiti tudi z namestitvijo tablete ob dlesen ali z vdihanjem peroralnega pršila, vendar je sublingvalna uporaba naj pogostejša. Dolgodelujoče nitrate je treba jemati od 1- do 4-krat nakoncentracijo holesterola, je treba zdraviti takoj. Kajenje je najpomembnejši preprečljivi dejavnik tveganja za to bolezen.
Zdravljenje angine pektoris je deloma odvisno od izrazitosti in stabilnosti simptomov. Če so simptomi stabilni in blagi do zmerni, utegne biti najučinkovitejša pot odpravljanje dejavnikov tveganja in uporaba zdravil. Če se simptomi hitro slabšajo, se zdravniki po navadi odločijo za takojšen sprejem bolnika v bolnišnico in za zdravljenje z zdravili. Če simptomi kljub zdravilom, dieti in spremembam življenjskega sloga ne popustijo občutno, pride v poštev angiografija, ki omogoča presojo o možnosti za obvodno operacijo ali angioplastiko koronarne arterije.
Zdravljenje nestabilne angine pektoris
Bolnike z nestabilno angino pektoris pogosto sprejmejo v bolnišnico, da natančno nadzirajo zdravljenje z zdravili in lahko uporabijo še druge načine zdravljenja, če je potrebno. Ti bolniki dobijo zdravila, ki zmanjšajo nagnjenost krvi k strjevanju. Predpišejo jim lahko tako heparin, antikoagulantno zdravilo, ki zavira strjevanje, kot acetilsalicilno kislino. Za zmanjšanje obremenitve srca dobijo tudi zaviralce beta in intravenski nitroglicerin. Ce zdravila niso učinkovita, utegnejo biti potrebne koronarna arteriografija in angioplastika ali obvodna operacija.
Obvodna operacija koronarne arterije: Takšna operacija (ki ji včasih pravijo tudi premostitvena ali »bypass«) je izredno učinkovita pri bolnikih z angino pektoris, pri katerih bolezen koronarnih arterij ni razširjena. Izboljša lahko zmožnost za telesne obremenitve, ublaži simptome in zmanjša število potrebnih zdravil ali njihovih odmerkov. Obvodna operacija bo najverjetneje koristila bolnikom s hudo angino pektoris, ki se ne izboljša po zdravljenju z zdravili, pa jim srce deluje normalno, še niso imeli srčnega infarkta in tudi nimajo drugih bolezni, zaradi katerih bi bila operacija tvegana (npr. kronične obstruktivne pljučne bolezni).
Video vsebina: Zdravljenje nestabilne angine in miokardnega infarkta.

Pri takšnih bolnikih je umrljivost ob neurgentni operaciji manj kot 1-od-stotna, nevarnost za okvaro srca (npr. za srčni infarkt) pa manj kot 5-odstotna. Približno 85 odstotkov bolnikov po operaciji nima več simptomov ali se jim ti močno ublažijo. Operacija je nekoliko bolj tvegana pri bolnikih, ki imajo zmanjšano črpalno zmogljivost srca (slabo delovanje levega prekata), srčno mišico okvarjeno zaradi predhodnega srčnega infarkta ali kakšne druge kardiovaskularne težave.
Obvodna operacija pomeni vstavitev venskega ali arterijskega presadka od aorte (glavne arterije, po kateri kri odteka iz srca po telesu) do koronarne arterije; presadek vodi mimo zoženega predela (obvod ali premostitev). Vene navadno vzamejo iz nog. Večina kirurgov kot presadek uporabi tudi vsaj eno arterijo. Po navadi jo vzamejo izpod prsnice.
Na teh arterijah se redko razvije koronarna bolezen. Več kot 90 odstotkov jih 10 let po operaciji še vedno dobro deluje. Venski presadki se lahko postopoma zožujejo. Po 5 letih jih je tretjina ali še več povsem neprehodnih. Poleg tega, da obvodna operacija izboljša simptome angine pektoris, nekaterim ljudem - zlasti tistim s hudo boleznijo - izboljša prognozo.
Razlogi za angioplastiko so pri bolnikih z angino pektoris podobni kot za obvodno operacijo. Za angiopla-stično zdravljenje pa niso primerne vse zožitve koronarnih arterij, in sicer zaradi svoje lege, dolžine, izrazitosti kalcifikacije in drugih okoliščin. Zato zdravniki skrbno ocenijo, ali je bolnik primeren kandidat za takšen poseg.
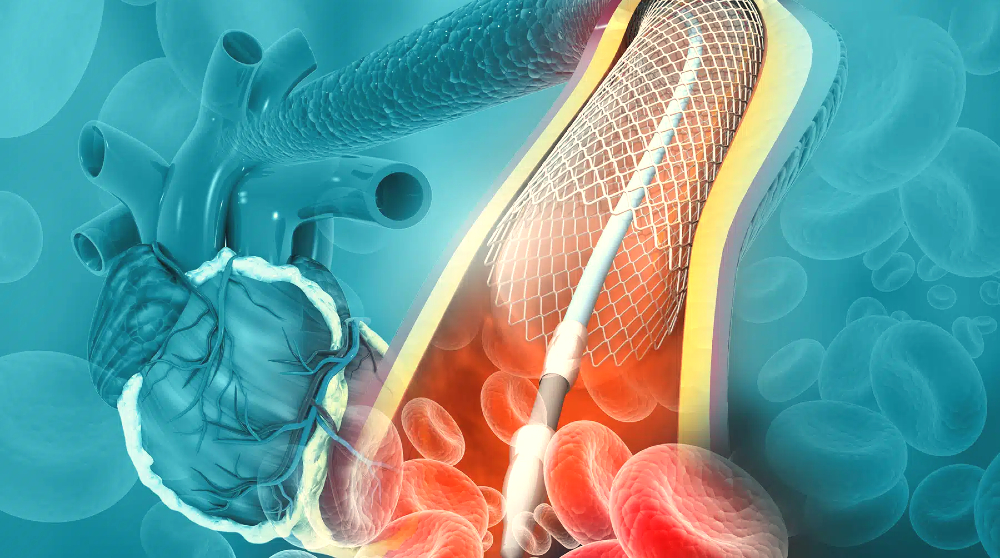
Zdravnik najprej zabode veliko iglo v veliko periferno arterijo, po navadi stegensko arterijo v dimljah. Skoznjo uvede dolgo vodilno žico v arterijski sistem, skozi aorto in v zoženo koronarno arterijo. Po vodilni žici v prizadeto koronarno arterijo vstavi kateter, ki ima na konici balon. Namesti ga tako, da je balon na mestu zožitve. Potem balon za nekaj sekund napihne. Napihovanje in izpihovanje je mogoče večkrat ponoviti.
Slika: Zdravniki uspešno odprejo od 80 do 90 odstotkov prizadetih arterij, ki jih dosežejo.
.jpeg)
Bolnika med posegom skrbno nadzirajo, ker napihnjenje balona za hip prekine pretok krvi skozi koronarno arterijo. Takšna zapora pri nekaterih ljudeh izzove EKG spremembe in ishemične simptome. Napihnjen balon stisne aterom, razširi arterijo in delno pretrga notranjo plast arterijske stene. Če je angioplastika uspešna, se obstrukcija močno zmanjša. Zdravniki uspešno odprejo od 80 do 90 odstotkov prizadetih arterij, ki jih dosežejo.
Med angioplastiko umre 1 do 2 odstotka bolnikov, od 3 do 5 odstotkov pa jih doživi neusoden srčni infarkt. Pri 2 do 4 odstotkih bolnikov je treba takoj po angioplastiki narediti obvodno operacijo. Pri približno 20 do 30 odstotkih se koronarna arterija v 6 mesecih spet zoži - pogosto se to zgodi že v prvih nekaj tednih po posegu.
Angioplastiko marsikdaj ponovijo in lahko dolgo časa uspešno obvladuje koronarno bolezen. Za preprečitev ponovne zožitve po angioplastiki lahko zdravnik uporabi novejši način, in sicer v arterijo vstavi žično mrežico, t. i. žilno opornico. Namestitev opornice po vsem sodeč prepolovi nevarnost poznejše arterijske obstrukcije.
Malo raziskav je primerjalo uspehe angio-plastike z uspehi zdravljenja z zdravili. Menijo, da je angioplastika približno enako uspešna kot obvodna operacija. V raziskavi, v kateri so obvodno operacijo primerjali z angioplastiko, se je pokazalo, da je bil po angioplastiki čas okrevanja krajši, umrljivost in nevarnost srčnega infarkta pa sta v dveh letih in pol, kolikor je trajala raziskava, ostali približno enaki.
Slika: Namestitev opornice po vsem sodeč prepolovi nevarnost poznejše arterijske obstrukcije.
Med novejšimi načini za odstranjevanje ateromov, od katerih številne šele preizkušajo, je tudi uporaba naprav za izvrtanje debelih, fibroznih in kalcificiranih sprememb. Toda ti načini obvodna operacija in anginoplastika so vselej mehanični posegi za odpravo neposredne težave in ne ozdravijo osnovne bolezni. Za izboljšanje splošne prognoze mora bolnik vplivati na dejavnike tveganja.
Vprašanja in odgovori
Kaj so najpogostejši vzroki za ravoj bolezni koronarnih arterij?
Koronarna bolezen nastane zaradi poškodbe notranje plasti koronarne arterije. Poškodbo lahko povzročijo naslednji dejavniki:
- kajenje
- visok krvni pritisk
- visoka raven holesterola
- diabetes ali odpornost na inzulin
- pasiven način življenja
- obsevalna terapija na področju prs[1]
Kako učinkovito je zdravljenje nestabilne angine pektoris?
Zdravljenje nestabilne angine pektoris je odvisno od posameznih okoliščin in resnosti stanja. Pomembno je, da se o vašem stanju in načrtu zdravljenja pogovorite s svojim kardiologom. Pravočasno in ustrezno zdravljenje lahko zmanjša tveganje za srčne zaplete.
Kako se diagnosticira angino pektoris?
Zdravnik diagnosticira angino pektoris predvsem po bolnikovem opisu simptomov. Med napadom značilne angine pektoris so po navadi opazne spremembe v EKG, v obdobjih med posameznimi napadi pa je lahko EKG normalen.
Ali je angina pektoris lahko smrtna?
Običajno ni življenjsko nevarna, vendar je opozorilni znak, da bi lahko bili v nevarnosti srčnega infarkta ali možganske kapi. Z zdravljenjem in spremembami zdravega načina življenja je angino pektoris mogoče nadzorovati in zmanjšati tveganje za resnejše težave[2].
Ali visok holesterol lahko privede do razvoja angine pektoris?
Angina (tako stabilna kot nestabilna) nastane, ko kateri koli vzrok povzroči zoženje koronarnih arterij. To lahko vključuje tudi visok holesterol[3].
Viri in reference
Veliki zravstveni priročnik za domačo uporabo, Založba mladinska knjiga
- Koronarna arterijska bolezen - https://www.humanitas.net
- Angina - https://www.nhs.uk
- Causes of angina - https://www.news-medical.net





 Facebook
Facebook
 Instagram
Instagram
 info@moja-lekarna.com
info@moja-lekarna.com

